
 Angioedema (or Quincke’s edema) is inflammation of the deep dermis or submucosa. It is non pitting, non dependent, non tender, non erythematous, usually assymmetric. The term angiioneurotic oedema was a misnomer as it was initially thought to be a nervous system disorder. It can be life threatening if it involves the airway. It can be congenital, idiopathic, or drug induced. Ace inhibitor blood pressure medications are common offenders causing this condition. NSAIDS and food allergies are the other big culprit. A thorough allergy history and testing are paramount. Exciting new drugs are on the horizon for this condition.
Angioedema (or Quincke’s edema) is inflammation of the deep dermis or submucosa. It is non pitting, non dependent, non tender, non erythematous, usually assymmetric. The term angiioneurotic oedema was a misnomer as it was initially thought to be a nervous system disorder. It can be life threatening if it involves the airway. It can be congenital, idiopathic, or drug induced. Ace inhibitor blood pressure medications are common offenders causing this condition. NSAIDS and food allergies are the other big culprit. A thorough allergy history and testing are paramount. Exciting new drugs are on the horizon for this condition.
Heinrich IrenaeusQuincke (26 August 1842 – 19 May 1922) was a German internist and surgeon who internist and surgeon. He was perhaps the first (1882) to recognize angioedema which is often referred to as “Quincke’s edema”.[1] “Quincke’s pulse”, with redness and pallor seen under the fingernails, is one of the signs of aortic insufficiency.“Quincke’s puncture” is a somewhat outdated eponym for lumbar puncture, used for the examination of the cerebrospinal fluid in numerous diseases such as meningitis and multiple sclerosis. In 1893 he described what is now known as idiopathic intracranial hypertension, which he labeled “serous meningitis”.
Discoveries
He was perhaps the first (1882) to recognize angioedema which is often referred to as “Quincke’s edema”.[1] “Quincke’s pulse”, with redness and pallor seen under the fingernails, is one of the signs of aortic insufficiency.[2] “Quincke’s puncture” is a somewhat outdated eponym for lumbar puncture,[3][4] used for the examination of the cerebrospinal fluid in numerous diseases such as meningitis and multiple sclerosis. In 1893 he described what is now known as idiopathic intracranial hypertension, which he labeled “serous meningitis”.[5]
 Congenital or Hereditary Angioedema is relatively rare. It usually shows up in childhood. It is essentially caused from either absent of non functioning complement factors. Primarily C1 Esterase Inhibitor. Acquired or hereditary angioedema do not typically respond to antihistamines or steroids, so the fact that he got better with these medications argues against this. It is bradykinin mediated and inflammation peaks in about 12 hours. Also, Hereditary Angioedema does not Urticate (No Hives). Nevertheless, checking labs would put these (remote) possibilities to rest. A good laboratory screen would be aC2, C3, C4, C1q, and C1-INH level and function, ESR, ANA, RF, hepatic transaminases, TSH, T4, anti-thyroglobulin antibodies, anti-thyroid peroxidase antibodies, CBC/diff and CU index (available thru Quest and Labcorp). If your patient has had a recent reaction, then simple doing a C4 assay will rule out a hereditary etiology. I have yet to diagnose a case of this. The drug company that manufactures cinryze is a human derived C1 esterase inhibitor and has to be given IV every few days and cost nearly 300k per year. Given androgens on a regular basis is the other option for this chronic condition.
Congenital or Hereditary Angioedema is relatively rare. It usually shows up in childhood. It is essentially caused from either absent of non functioning complement factors. Primarily C1 Esterase Inhibitor. Acquired or hereditary angioedema do not typically respond to antihistamines or steroids, so the fact that he got better with these medications argues against this. It is bradykinin mediated and inflammation peaks in about 12 hours. Also, Hereditary Angioedema does not Urticate (No Hives). Nevertheless, checking labs would put these (remote) possibilities to rest. A good laboratory screen would be aC2, C3, C4, C1q, and C1-INH level and function, ESR, ANA, RF, hepatic transaminases, TSH, T4, anti-thyroglobulin antibodies, anti-thyroid peroxidase antibodies, CBC/diff and CU index (available thru Quest and Labcorp). If your patient has had a recent reaction, then simple doing a C4 assay will rule out a hereditary etiology. I have yet to diagnose a case of this. The drug company that manufactures cinryze is a human derived C1 esterase inhibitor and has to be given IV every few days and cost nearly 300k per year. Given androgens on a regular basis is the other option for this chronic condition.
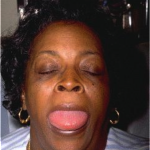 The vast majority of Angioedema is idiopathic and often drug induced. It is essentially a deeper (subdermal or submucosal) version of urticaria and is similarly most often idiopathic. It usually manifests in adulthood. Medications started within the past several months are most likely. However, ACE inhibitors are notorious for causing these reactions even after years of safe use. Aspirin and NSAIDs are also frequent causes or exacerbating factors. Less commonly, underlying problems like thyroid disease, liver disease, autoimmune disease or occult malignancy can be responsible. About half of patients with otherwise “idiopathic” chronic urticaria/angioedema make IgG autoantibodies against the high affinity IgE receptor on mast cells. Foods are uncommon offenders, but should be considered. Routine allergy testing and diet diary are appropriate. Non hereditary forms are histaminic and thus respond better to allergy medications such as antihistamines, epinephrine, and steroids.
The vast majority of Angioedema is idiopathic and often drug induced. It is essentially a deeper (subdermal or submucosal) version of urticaria and is similarly most often idiopathic. It usually manifests in adulthood. Medications started within the past several months are most likely. However, ACE inhibitors are notorious for causing these reactions even after years of safe use. Aspirin and NSAIDs are also frequent causes or exacerbating factors. Less commonly, underlying problems like thyroid disease, liver disease, autoimmune disease or occult malignancy can be responsible. About half of patients with otherwise “idiopathic” chronic urticaria/angioedema make IgG autoantibodies against the high affinity IgE receptor on mast cells. Foods are uncommon offenders, but should be considered. Routine allergy testing and diet diary are appropriate. Non hereditary forms are histaminic and thus respond better to allergy medications such as antihistamines, epinephrine, and steroids.
Treatment is largely symptomatic. Symptoms wax and wane for weeks and even months. Unfortunately up to 95% of patients will never find the etiology. I often suggest a daily 24 hour acting antihistamine to prevent/suppress episodes, such as Zyrtec 10 mg qd. If symptoms persist, you can add Allegra 180 mg qam and take Zyrtec 10 mg qhs. If symptoms STILL persist, you can continue Allegra and switch Zyrtec to Atarax, titrated as needed to suppress episodes while minimizing (hopefully) daytime sedation. I also often add a type 2 antihistamine such as Zantac. Steroids of course are helpful, however one should be cautious of rebound inflammation.