AIRWAY & LARYNGOLOGY—-DANIEL TODD, MD
IF YOU GET A CALL EVEN REMOTELY CONCERNING THE AIRWAY—-YOU MUST SEE THE PT—FAIRLY SOON
IF YOU ADMIT A PT TO WATCH THEIR AIRWAY—YOU HAD BETTER SECURE IT
NO ONE IS GOING TO TELL YOU WHEN THE PT NEEDS A TRACH BUT THERE ARE PLENTY OF FOLKS AROUND TO TELL YOU WHEN YOU NEEDED ONE——IT IS CERTAINLY EASIER TO DEFEND A CONTROLLED INTUBATION OR TRACH SCAR THAN A DEAD PT
EMERGENCY
AIRWAY
AIRWAY IS FIRST BUT NEVER AT THE EXPENSE OF THE C-SPINE
EVERY PT YOU SEE IN A TRAUMA SITUATION SHOULD BE ON A SPINE BOARD WITH AN IMMOBILIZING PHILLIE COLLAR–IF THEY ARE NOT IMMEDIATELY QUESTION THE MANAGEMENT
PROBABLY STILL BEST WAY TO ESTABLISH AN AIRWAY IN THE FACE OF C-SPINE INJURY IS OROTRACHEAL INTUBATION FOLLOWING NEUROMUSCULAR BLOCKADE (ONCE THE PATIENT IS PARALYZED YOU HAVE ONLY ONE OPTION) AND INLINE CERVICAL STABILIZATION—-BE READY FOR A CRIC OR A TRACH
CRICOTHYROIDOTOMY (EMERGENT CONIOTOMY)—FOR ADULTS ONLY—CHILDREN LESS THAN 8 GET NEEDLE CRICOID WITH NASAL CANULA O2 WIDE OPEN (10 LITERS)—-EMERGENT TRACH IS DANGEROUS—CRIC LEADS TO SIG INCIDENCE OF POST OP SUBGLOTTIC STENOSIS AND SCARRING
FIRST GET READY FOR CRIC(NEVER GET CRITICIZED FOR PERFORMING A CRICOTHYROTOMY)
INJECT FOR HEMOSTASIS AND ANESTHESIA IF POSSIBLE
10 BLADE–LARGE HORIZONTAL 0R VERTICLE INCISION
SUCTION
TRACH SPREADER-LARGE NASAL SPECULUM—-OR LARGE KELLY/GOLD/CRILE
CRIC HOOK
CLAMPS
ETT TUBE
SURGICEL
RSI (RAPID SEQUENCE INTUBATION)
PEDS–LARGER OCCIPUT, LARGER TONGUE, SMALLER EPIGLOTTIS, HIGHER MORE ANT LARYNX, SHORTER AND NARROWER TRACHEA—-TRACHEA— ”ARTERIA TRACHEA”=ROUGH ARTERY—ERISISTRATUS OF CHIOS=THE FOUNDER OF PHYSIOLOGY—ALEXANDRIAN SCHOOL 300 BC
ALWAYS CONSIDER AN ENDOSCOPICALLY GUIDED NASO OR ORO TRACHEAL INTUBATION—EASY WHEN PLANNED
Hx–AMPLE
ALLERGIES
MEDS
PMHx
LAST MEAL
EXISTING CIRCUMSTANCES
PREP EQUIPMENT—O2, LARYNGOSCOPE, SUCTION, ETT(PINKY SIZE), BVM, PULSE OX, MONITOR, DRUGS, ET CO2 DETECTOR, LMA, SURGICAL AIRWAY STUFF—PEDS ETT (PINKY FINGER OR AGE/4 + 4) SIZING
PREOXYGENATE—-NITROGEN WASHOUT
MEDICATE—RELAX, SEDATE, PARALYZE(VERSED, SUCC, FENTYNYL)
POSITION PT—-KILLIANS FLEXION-FLEXION AFFORDS THE BEST VISUALIZATION—–>> SNIFFING POSITION (BOYCE-JACKSON SNIFFING POSITION (FLEXION OF THE NECK TO CHEST AND EXTENSION OF THE HEAD TO NECK)—–THE LARGE OCCIPUT IN YOUNG PEDS PRECLUDES THE NEED FOR A PILLOW.——–EXTENSION-EXTENSION WITH THE KILLIANS SUSPENSION LARYNGOSCOPE REQUIRES BRUNNINGS EXTERNAL COUNTERPRESSURE DEVICE.
SELLICK MANEUVER (PREVENT ASPIRATION AND HELP POSTERIORIZE LARYNX)
SUCTION AND INTUBATE–IF YOU MISS—CONSIDER LEAVING THE 1ST TUBE IN THE ESOPHAGUS AS A REFERENCE
CAN USUALY INTUBATE THE NEONATE WITH NO SEDATION—EASY TO OVER POWER—-A 2.5 MM ETT IS THE SMALLEST YOU CAN SUCTION WITH—-RECALL THAT LESS THAN 3.5 MM DIAMETER OF THE SUBGLOTTIS IS BY DEFINITION STENOSIS
LARYNGOSPASM/INVOLUNTARY MUSCLE CONTRACTION—STAGE II OF GENERAL ANESTHESIA
POSITIVE PRESSURE VENTILATION HELPS HOLD THINGS OPEN—-GET AN AMBU BAG
ALWAYS CONSIDER AN LMA—BUYS YOU TIME—-CAN INTUBATE THROUGH A #4-5 LMA WITH A FLEXIBLE SCOPE AND A SMALL #7 NASAL TUBE
CONSIDER A RIDGID BRONCH AS WELL
URGENCY
LARYNGEAL TRAUMA—A LITTLE TIME–TRY TO TRACH
GET FLEXIBLE SCOPE
LOCAL TRACHEOTOMY—ALWAYS PREFERRED OVER A CRIC—-SAVES YOU HEAD ACHES–BUT NEED SOME TIME
INJECT LOCAL—IV SEDATION(VERSED)
DO A VERTICAL SLIT INCISION INTO THE TRACHEA IN PEDS TO AVOID LONG TERM COMPLICATIONS
TRACHEOTOMY TRAY
BOVIE FROM THE OR
SUCTION
HEADLIGHT
TRACH TUBE
HORIZONTAL INCISION?
CRIC HOOK—BRING IT TO YOU
ENTER TRACHEA—-DO A VERTICAL SLIT INCISION IN PEDS TO AVOID LONG TERM COMPLICATIONS
PROBABLY IN ALL PEDS < 5 YEARS DO A VERTICLE SKIN INCISION AND STAY TOTALLY MIDLINE TO AVOID A PNEUMO—–MAY BENEFIT FROM LOOPS
GET POST PROCEDURE CXR—-HIGH INCIDENCE OF PNEUMO WITH PEDS AND COPD(HIGH PLEURAL DOMES) AND WITH EMERGENT OR DIFFICULT TRACHS—-S.Q. AIR IS A WARNING SIGN—-ALSO SEE PNEUMOMEDIASTINUM
HIGH INCIDENCE OF TENSION PNEUMOTHORACIES WHEN USING A JET VENTILATOR—MANIFEST AS A MARKEDLY INCREASED COMPLIANCE
AFTER ESTABLISHING RESP SUPPORT—CONSIDER CIRCULATION/VOLUME STATUS—GET IV (3 TRIES IN 90 SECONDS—THEN INTRAOSSEOUS) ACCESS GIVE LR OR NS 20 MG/KG BOLUSES—-CONSIDER GLUCOSE STATUS (D5NS)
IF YOU ANTICIPATE A DIFFICULT AIRWAY POST OP–EXTUBATE OVER A TUBE GUIDE
CONTRAINDICATIONS FOR BLIND NASOTRACHEAL INTUBATION = OSA AND FACIAL FRACTURES (COULD HAVE FX OF SKULL BASE)
STERTOR=NP TURBULENCE—–OFTEN DIFFICULTY FEEDING—DEFINED IN SOME PLACES AS A SYNONYM FOR SNORING?
INFANTS = OBLIGATE NASAL BREATHERS UP TO ABOUT 8 WEEKS (SOME LONGER)— -CYCLICAL CYANOSIS WITH NASAL OBSTRUCTION
ORO- OR HYPOPHARYNGEAL OBSTRUCTION (OFTEN DUE TO ADENOTONSILLAR HYPERTROPHY =/- HYPOTONIA)—-PRODUCES GURGLING UPPER AIRWAY NOISES, DYSPHAGIA, AND OFTEN INSP OBST. (OSA) AND SNORING--FULL OR MUFFLED VOICE, ASSOC. DROOLING, FEEDING DIFFICULT
STRIDOR = NOT A BENIGN SIGN OR A FINAL DIAGNOSIS—FEEDING USUALLY NL
MUST TAKE A GOOD HISTORY—-ABNL PHONATION, DYSPHAGIA?
WORSE WHEN SLEEPING—PROBABLE PHARYNGEAL HYPOTONIA
WORSE WHEN AWAKE/AGITATED—PROBABLY PARALARYNGEAL
INSP “WET”=SUPRA OR GLOTTIC-(EXTRATHORACIC)–OFTEN APHONIC OR HOARSE (PROLONGED INSP PHASE—DIFFICULTY INSPIRING)—–SHALLOW INSP SLOW VOLUME ON PFTS
THE SAME VOLUME OF AIR IS MOVED DURING INSP AND EXP—-BUT INSP IS ONLY 1/3RD THE LENGTH SO MORE V0LUME IS MOVES PER UNIT TIME
BIPHASIC(TWO WAY STRIDOR) “CROWDING” =SUBGLOTTIC OR MIDTRACHEAL–OFTEN BARKING COUGH WITH NL VOICE—-INITIALLY INSP AND THEN EXP—–USUALLY REPRESENTS A FIXED OBSTRUCTION—-SHALLOW INSP AND EXP FLOW VOLUME LOOPS ON PFTS
INSP IS USUALLY MORE SIGNIFICANT
EXP(SONOROUS) “WHEEZING”=DISTAL TRACHEOBRONCHIAL TREE (MAY ALSO HAVE ASSOC. WHEEZING)–BRASSY COUGH (PROLONGED (DIFFICULT) EXPIRATORY PHASE—-SHALLOW EXP FLOW VOLUM LOOP
NL PARTY WALL/MEMBRANOUS TRACHEA PULLS OPEN DURING INSPIRATION–NEG INTRATHORACIC PRESSURE—SO TRACHEA IS LARGER ON INSP AND SMALLER ON EXP WHERE THE TURBULENT AIRFLOW IS HEARD
ANY LEVEL OF OBSTRUCTION CAN HAVE BIPHASIC STRIDOR IF IT IS SEVERE ENOUGH
DECREASING STRIDOR OFTEN HERALDS FATIGUE AND IMPENDING DECOMPENSATION
TACHYPNEA(RR) + HYPERNEA(TV) = HYPERVENTILATION(MINUTE VENTILATION)–REPRESENTED BY Pco2
RR > 80 SIG IN NEONATE OR CHILD
HYPOXIA–PaO2 < 50
CYANOSIS=>5MG/DL DEOXYHb (SEVERELY ANEMIC PT CANNOT DEMONSTRATE CYANOSIS)
POOR AIR EXCHANGE (DYSPNEA, GRUNTING, FLARING, RETRACTIONS)
BOURNOULLI PRINCIPLE=VENTURI PRINCIPLE(VENTURI TUBE)–HIGH VELOCITY FLOW RELATES TO LOW LATERAL PRESSURE–LOOSE SUBMUCOSA, SWELLING AND LOW LATERAL PRESSURE CAN ACT TO DECREASE THE DIAMETER OF THE AIRWAY
ONE UNIT OF DECREASED RADIUS LEADS TO A 4 FOLD INCREASED RESISTANCE
1MM OF SWELLING LEADS TO A 35% REDUCTION IN CIRCUMFERENCE, A 16 FOLD INCREASE IN RESISTANCE, AND A 75% DECREASE IN THE CROSS SECTIONAL AREA IN THE NEONATE——LESS SEVERE IN THE OLDER PT
INTENSITY (AMPLITUDE) IS PROPORTIONAL TO THE FLOW VELOCITY
FREQUENCY IS PROPORTIONAL TO THE DIAMETER OF THE LUMEN
AGITATION IS SECONDARY TO HYPOXIA UNTIL PROVEN OTHERWISE—-SEDATION ONLY LOWERS THE RESPIRATORY DRIVE
LETHARGY AND CYANOSIS ARE LATE SIGNS OF HYPOXIA—–WHEN THEY TELL YOU THE PT WAS REALLY STRUGGLING BEFORE BUT HE HAS CALMED DOWN NOW—–THE PT IS REALLY JUST GETTING READY TO GIVE UP AND DIE!!
Hx
AGE OF ONSET : BIRTH—CONG SUBGLOTTIC STENOSIS, LARYNGOMALACIA, VOCAL CORD PARALYSIS, CHOANAL ATRESIA
SEVERAL MONTHS OF AGE—SUBGLOTTIC HEMANGIOMA
LATE INFANCY–ORO- AND HYPOPHARYNGEAL COLLAPSE (WHEN METABOLIC DEMANDS INCREASE)
TODDLERS—F.B. ASPIRATION, CROUP, EPIGLOTTITIS, TRACHEITIS
CHILDHOOD—ADENOTONSILLAR HYPERTROPHY, BACTERIAL TRACHEITIS
DURATION, POSITIONAL, SLEEPS WELL, DIFFICULTY FEEDING, WEIGHT GAIN, VOICE, CRY, PROGRESSION, ASSOC. URI, COUGH, DYSPHAGIA, ONDYNOPHAGIA, ASTHMA, FOREIGN BODY, TRAUMA, LAST P.O., MEDS, ALLERGIES, PMHx, HISTORY OF INTUBATION, GROWTH AND DEV. (4 YRS, 40 IN, 40 LBS)
SPECS ( SEVERITY OF PROBLEM, PROGRESSION, EATING DIFFICULTY, CYANOSIS OR APNEA, SLEEP IMPACT)
PE
CRANIOFACIAL ABNL?
AUSCULTATE, LOOK AT PTS COLOR, CHECK PULSE OX AND ABG, LOOK AT POSITION PT ASSUMES (LARYNGOMALACIA MAY ASSUME PRONE POSITION WHILE SUPRAGLOTTITIS OFTEN LEAN FORWARD, RESP DISTRESS–RETRACTIONS(SUBCOSTAL, INTERCOSTAL), CYANOSIS, NASAL FLARING, HTN, TACHY(>180), RR, FEVER, DROOLING, VOMITING
HIGH KILOVOLTAGE LAT NECK RADIOGRAPHS—EPIGLOTTIS AND HYOID MAKE AN “X”–CAN SEE VENTRICLE, CXR!
XERORADIOGRAMS
CXR
CT OF NECK AND CHEST
FLEXIBLE ENDOSCOPIC EXAM
MBLE(MICROSCOPIC BRONCHOSCOPY LARYNGOSCOPY AND ESOPHAGOSCOPY)–NEONATES–MAY DO COLD WITH NOSEDATION OR ANESTHETIC (JUST TOPICAL LIDO)—EASY INTUBATION AND CONTROL–THEY USUALLY DO NOT COMPLAIN—INFANTS MAY TAKE P.O. FLUIDS UP TO 2 HOURS PRE-OP—HELPS MAINTAIN GLUCOSE HEMOSTASIS—–VERSED 0.5-0.75 MG/KG P.O. IN KOOLAID 20 MIN OCOR—NITROUS, O2 AND HALOTHANE—-THEN UNDERSEDATION START IV AND GIVE ROBINOL 0.01MG/KG IM AFTER ANESTHETIC—MORE POTENT ANTISIALOGOGUE AND DOES NOT CROSS BBB AND GIVES LESS TACHY THAN ATROPINE—OBSERVE SPONT B TVC MOTION—SPRAY CORDS WITH LIDOCAINE, PALPATE ARYTENOIDS FOR MOBILITY —ALWAYS CHECK FOR PLC—90 DEGREE PROBE, PH PROBE, ESOPHAGOSCOPY, MOD BARIUM SWALLOW, EKG, ABG, FEES—–MAY WANT TO CALIBRATE AIRWAY SIZE WITH DIFFERENT ETT’S
MRI—HIGH SUSPICION OF COMPRESSIVE VASCULAR LESIONS
LABS: MHATP, THYROID PROFILE, ANT NARES CULTURE, REFLUX EVAL
CAVEATES:
ONLY LEAVE PTS INTUBATED 7-10 DAYS (MAX = 2 WEEKS)—–COMPLICATIONS INCREASE EXPONENTIALLY AFTER 7 DAYS
AVOID NG TUBES WITH ETT—-CAUSES UNDUE ARYTENOID IRRITATION
PERC GASTROSTOMY IS A GOOD OPTION
FREQUENT MANOMETRIC TESTING OF THE BALLOON
USE SAME MIXTURE OF GASSES ANESTHESIA IS USING TO FILL THE BALLOON(NITROUS OXIDE CAN ELEVATE PRESSURES AND LEAD TO AN ISCHEMIC NEUROPRAXIA OF THE ANT BR OF THE RLN
THERE ARE EXPENSIVE FOAM FILLED CUFFS—NEED TO BE EVACUATED Q 8 HOUR—THE CUFF PRESSURES CAN BE SYNCHRONIZED TO THE VENTILATOR
ADJUST CHILD’S HEAD POSITION AT REGULAR INTERVALS TO MOVE THE PRESSURE POINT OF THE UNCUFFED TUBE
SELECT THE SIZE OF THE ETT BASED ON LEAN-BODY MASS—NOT APPEARANCE
USE BIOCOMPATIBLE ETT
PLACE CUFF 6-10 MM BELOW THE GLOTTIS—FIX IN TO PREVENT MIGRATION
LEAKS AROUND THE CUFF ARE NOT DUE TO THE SIZE OF THE TRACH TUBE BUT THE SHAPE OF THE TUBE AND ITS RELATIVE POSITIONING—MAY TRY AN EXTRALENGTH TUBE—TIGHTEN THE COLLAR—PACK AROUNT THE PROXIMAL FLANGES OVER THE SKIN—-IF NONE OF THESE WORK MAY ORDER A SOFT TRACH (EXPENSIVE)
A MUCOUS PLUG WHICH PRESENTS WITH DECREASED VENTILATION (POOR COMPLIANCE, HIGHER PRESSURES, DECREASED O2 AND INCREASED CO2) MAY TAKE AN HOUR TO SHOW UP RADIOGRAPHICALLY—USUALLY HERALDS THE ONSET OF PNEUMONIA
ENTITIES:
LARYNGEAL INFXNS
 ACUTE EPIGLOTITIS/SUPROGLOTITIS = OEDEMA GLOTTIS = SUPRAGLOTTIC CROUP
ACUTE EPIGLOTITIS/SUPROGLOTITIS = OEDEMA GLOTTIS = SUPRAGLOTTIC CROUP
NO COUGH
AGE 2-7 (CHECK IMMUNE STATUS)—-BECOMING ADULT DISEASE
IN ADULTS—MORE OF A SUPRAGLOTTITIS—THINK ABOUT A POSSIBLE ETIOLOGY OTHER THAN BAD LUCK—-F.B. OR CA
EPIGLOTTIC ABSCESS (PRIMARILY S.A.) IS RARE —SO REALLY BE SUSPICIOUS ABOUT AN UNDERLYING PROBLEM
NOT ALWAYS DUE TO H. INF TYPE B (STREP PNEUMO AND S.A. ARE MOST COMMON IN ADULTS)
DECREASED 85% SINCE THE CONJUGATED VACCINE
BEST IS T-CELL DEP RESPONSE TO THE CONJUGATE VACCINE
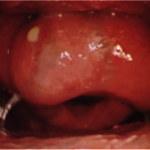
CHERRY RED EPIGLOTIS
 “THUMB PRINT SIGN” ON LAT SOFT TISSUE NECK FILM—–OMEGA SHAPED EPIGLOTTIS MAY MIMIC THIS
“THUMB PRINT SIGN” ON LAT SOFT TISSUE NECK FILM—–OMEGA SHAPED EPIGLOTTIS MAY MIMIC THIS
FAST ONSET(HOURS) — SPEED OF ONSET TENDS TO REFLECT Px–WITHIN 24 HOURS–SUBMUCOSAL INFXN
RAPID PROGRESSION
HOARSENESS
DROOLING –INABILITY TO HANDLE OWN SALIVA
LEANING FORWARD—EPIGLOTTIS TENDS TO SWELL ON ITS LINGUAL ASPECT AND PUSH POST—-MUCOSA IS TIGHTLY ADHERED TO LARYNGEAL SURFACE AND LOOSELY TO LINGUAL SURFACE
CAN OBSTRUCT AT ANY MOMENT
CAVEATE—NEVER COMFORTABLE IN A SUPINE POSITION AND RARELY A COUGH
DYSPHAGIA/ODYNOPHAGIA
FEVER
LARYNGEAL SARCOID MAY APPEAR THE SAME WITHOUT THE TOXICITY
Rx: OROTRACHEAL INTUBATION IN THE OR—-BE PREPARED TO DO A TRACH—CAN CHANGE OVER TO A NASOTRACHEAL TUBE IN THE OR—USUALLY NEED TO BE INTUBATED ABOUT 72 HOURS
ADULTS YOU CAN INTUBATE AND LEAVE SEDATED IN THE UNIT FOR A COUPLE OF DAYS—IF YOU HAVE A GOOD UNIT—OTHERWISE TRACH
IV ABX—ROCEPHIN/CEFUROXIME/CEFOTAXIME (30% AMP RESISTANT)
BLOOD CULTURES AND TARGETED ABX IF POSSIBLE
IV STEROIDS (DECADRON 1 MG/KG UP TO 15)—-MIGHT HOLD THIS UNTIL YOU KNOW YOU ARE COVERED
IVF
SUCTION
LARYNGITIS
ACUTE-–USUALLY VIRAL, TREAT SYMPTOMATICALLY–HYDRATION, VOICE REST. SECONDARY BACTERIAL INFXN (GABHS). RARELY DIPTHERIC LARYNGITIS—INSIDIOUS, HOARSE, CROUPY COUGH, GREY-WHITE MEMBRANE(UNDERLYING BLEEDING WHEN YOU REMOVE)–Rx: ERYTHROMYCIN OR PCN G, ANTITOXIN, TRACH (TOXIN AFFECTS CARDIAC AND NEURAL TISSUES)
CHRONIC-–TB, SYPHILITIC, RHINOSCLEROMA, HISTO, BLASTO, AND OTHER MYCOTIC INFXNS—–RARE IN IMMUNOCOMPETENT INDIVIDUALS
CROUP–ACUTE LARYNGEAL-TRACHEO-BRONCHITIS (LTB)–SUBGLOTTIC EDEMA
COUGH PRESENT
EPIGLOTTIS NOT INVOLVED-TVC’S VARIABLY INVOLVED—VOICE BECOMES HOARSE AS INFXN PROGRESSES
INFXN OF THE CONUS ELASTICUS (SUBGLOTTIC INTRINSIC LIG)
6 MONTHS – 5 YEARS OLD ( 1-3 YEARS)—-HOLINGER SAYS “ THERE IS NO SUCH THING AS CROUP UNDER 1 YEAR OF AGE!”
MALE > FEMALE
MORE IN WINTER
PRIMARILY VIRAL ( PARAINFLUENZA TYPE 1=MOST COMMONTHEN 2 – 4)/SECONDARY– -RSV—HAS A REMARKABLE PROPENSITY FOR THE SUBGLOTTIS AS WELL AS BRONCHIOLES (RSV BRONCHIOLITIS—-RIBAVIRIN)
?10-15% BACTERIAL — H. INF. STREP, MYCOBACTERIUM–STEVEN’S JOHNSON
STARTS AS URTI—CROUPY COUGH (“BRASSY” SEAL BARK COUGH)
DANIEL BOURNOULLI (1700) PRINCIPLE LEADING TO SUBGLOTTIC VIBRATIONS
BIPHASIC OR INSP. STRIDOR, LABORED BREATHING, INTERCOSTAL RETRACTIONS
PROBABLY DO NOT INTUBATE—IF YOU NEED TO USE THE SMALLEST TUBE NESCESSARY TO AVOID SUBGLOTTIC STENOSIS
LAT SOFT TISSUE X-RAY = 30% + “STEEPLE SIGN”
PROBABLY ADMIT—-A LOT TO LOSE (VARIABLE RECOMMENDATIONS IN THE LITERATURE)
O2
ULTRASONIC HUMIDIFICATION–TO AID IN THE EXPECTORATION OF INSPISSATED SECRETIONS AND CRUSTS
COOL AIR HELPS BY STIMULATING VASOCONSTRICTION AND REDUCING EDEMA
RACEMIC EPI (PRN ONLY—GET TACHYPHYLAXIS)
P.O. STEROIDS (PRELONE)—-TASTE TERRIBLE—PROBABLY A GOOD IDEA TO AVOID HOSPITALIZATION
NO SEDATION
POSSIBLY NEBULIZED STEROIDS ARE OF SOME BENEFIT
PROBABLY ANTIBIOTICS ARE BENEFICIAL FOR PROPHYLAXIS?
IF YOU NEED AN AIRWAY—PROBABLY TRACH
(VS PERTUSSIS—-WHOOP WITH TACHYPNEA AND CYANOSIS)
THE NEOPHYTE CLINITION SHOULD ALWAYS ERR ON THE SIDE OF CONSERVATISM)
TRANSIENT REACTIVE EDEMA OF THE CONUS ELASTICUS FOLLOWING GETA—SOUNDS LIKE CROUP
BACTERIAL TRACHEITIS= MEMBRANOUS LBT (MLBT) = BACTERIAL CROUP = PSUEDOMEMBRANOUS CROUP = NONDIPTHERITIC LARYNGITIS
USUALLY FROM PROGRESSION OF CROUP– A SUPERINFXN
> 50% STAPH AREUS, 2ND H. INF
USUALLY OLDER CHILDREN(AGE 8-12)
SEEMS TO BE A Q 20 YEAR EPIDEMIC
PURULENT CRUSTS
CXR -”SCALLOPING” OF THE TRACHEAL WALLS
RIDGID BRONCH WITH LAVAGE—-REMOVE CRUSTS
MAY KEEP PT INTUBATED BUT OFTEN TRACH IS INDICATED
NEED VERY GOOD PULM TOILET AND IV ABX
RRP (RECURRENT RESPIRATORY PAPILLOMATOSIS)
PRIMARILY HPV 6 & 11 (RARELY TYPE 16 & 18)
HIGH CORRELATION WITH MATERNAL HPV (CONTROVERSIAL TO CONSIDER C-SECTION)
MAY PROGRESS TO SCCA—SEEM THIS
REQUIRE MULTIPLE SURGERIES—CO2 VS PIPE—-BEST ITITIAL THERAPY IS CO2 LASER RESECTION
ADJUNCTIVE THERAPY REMAINS UNPROVEN—-MTX, RIBAVARIN, MUMPS, RETINOIDS—-RT?
TRACH —-AVOID IT IF YOU CAN TO AVOID DISTAL SEEDING
NEW DATA SEEMS EXCITING WITH INTRALESIONAL CIDOPIVIR/CIDOFOVIR–DONE THIS WITH GOOD RESULTS WITH 27 GUAGE NEEDLE
NON-INFECTIOUS (CONGENITAL, TRAUMATIC, NEOPLASTIC) ETIOLOGIES:
ANTERIOR CHOANAL STENOSIS
OFTEN ASSOC WITH A SINGLE INCISOR ON X-RAY(CT SCAN)
DRILL OUT THROUGH A SUBLABIAL APPROACH AND STENT
NASOLACRIMAL DUCT CYSTS—–MARSUPULIZE
Congenital posterior choanal atresia is an uncommon anomaly which can have life‑threatening consequences. The first recorded description of this disorder was by Otto in 1830. The first attempted repair was by Carl Emmert in 1851. The first recorded successful repair on an infant was in 1872 by Jacob Da Silva Solis‑Cohen. The transpalatal approach was first described by Brunk in 1909.
CAN BE MIMICKED BY MARKED NASAL MUCOSAL SWELLING (URTI/RHINITIS MEDICAMENTOSA)
1/7,000
FEMALE 2:1
UNILAT > BILAT
RIGHT SIDE 2:1
90% BONEY, 10% MEMBRANOUS = OLD DOGMA—-REALLY MOST ARE MIXED
CAN BE FAMILIAL
CAN BE POTENTIALLY LETHAL IF B——OBLIGATE NASAL BREATHERS UP UNTIL 6-8 WEEKS
50% OF UNILAT AND 75% OF BILAT ASSOC. WITH OTHER CONG ANOMALIES (20 X HIGHER RISK OF CONG. HEART DISEASE)
ASSOC. WITH APERT, TREACHER COLLINS, TRISOMY D, CHARGE SYNDROME
HIGH RATE OF DISCONGUGATE PHARYNGOLARYNGOMALACIA—-GERD AND OSA
COLOBOMA OF IRIS AND RETINA
HEART DEFECTS
ATRETIC CHOANAE
RETARDED DEVELOPEMENT—-BOTH PHYSICAL AND MENTAL
GENITAL HYPOPLASIA
EAR ANOMALIES
Dx: UNILAT NAO, PURULENT DRAINAGE, INABILITY TO PASS 6 FRENCH CATHODER AT DELIVERY—-USED TO PASS GENTIAN VIOLET OR METHYLENE BLUE OR IODIZED OIL AND GET CROSS TABLE LATERAL X-RAY—-NOW DO ENDOSCOPY
GET THIN CUT CT (NON-CONTRAST) OF THE NP IN THE PLANE OF THE PALATE
Rx: IMMEDIATE MCGOVERN ORAL NIPPLE TO ESTABLISH ORAL AIRWAY—TRACH LESS THAN 10% OF THESE PTS
GAVAGE FEEDINGS
GENERALLY DO NOT OPERATE UNLESS SYMPTOMATIC (OR BILAT)
CAN REPAIR TRANSNASAL (MICRODEBRIDER), TRANS-SEPTAL, TRANS-PALATAL, TRANS-ANTRAL—-+/- STENTING
LARYNGOMALACIA
DO FLEXIBLE EXAM—2 PASEES THROUGH THE NOSE
NEED TO SEE NL VOCAL CORD MOTION!
MOST COMMON CAUSE OF INFANTILE STRIDOR–>60% OF LARYNGEAL PROBLEMS IN INFANTS
A HARSH INSP STRIDOR– -WORSE WITH AGITATION—SEEMS TO ABATE WITH SLEEP (DO NOT GET SLEEP STUDY–ALTHOUGH HYPOTONIA MAY ALSO CONTRIBUTE TO OSA), POOR FEEDING–FTT—MUST MONITOR WEIGHT!, WORSE WITH AGITATION, WORSE SUPINE, WORSE EXTENDING THE HEAD, BETTER PRONE, BETTER FLEXING THE HEAD
FLACCID SUPRAGLOTTIC STRUCTURES–NO DIFFERENCE IN CARTILAGE- -NOT MORE COMMON IN PREMIES–THOUGHT TO BE THE RESULT OF HYPOTONIA/FLACCIDITY OF SUPRAGLOTTIC STRUCTURES
LONG OMEGA SHAPED EPIGLOTTIS—OMEGA SHAPE ALLOWS THE ARYTENOIDS TO FALL IN CLOSER TO THE MIDLINE, LARGE ARYTENOIDS AND CUNEIFORMS WITH REDUNDANT MUCOSA, FORESHORTENED A-E FOLDS—–A LOT OF POST/LAT COLLAPSE CORRELATES WELL WITH THE NEED FOR AN ENDOSCPOPIC SUPRAGLOTTOPLASTY!
REALLY 4 SUBTYPES
GENERALLY ONSET WITHIN FIRST 4-6 WKS (2-6 WEEKS) AFTER BIRTH(OFTEN FIRST 10 DAYS)—USUALLY PROGRESSES SOME UP TO 6 MONTHS AND THEN ABATES–PRIMARILY RESOLVES BY AGE 2
75% ASSOC, GERD—SO TREAT IT!, HYPOTONIA ASSOC WITH OSA—?T&A—-ALSO ASSOC WITH FTT
UP TO 5% INCIDENCE OF SURGICALLY TREATABLE 2ND AIRWAY ANOMALY—ARGUMENT FOR RIDGID ENDOSCOPY
Rx: OBS, CPAP,ENDOSCOPIC SUPRAGLOTTOPLASTY IF NECESSARY(5-10%)—ERRONOUSLY CALLED EPIGLOTTOPLASTY IN PAST–REALLY JUST CUT THE A-E FOLDS—RELEASE THEM(LASER OR COLD STEEL)—IF REFRACTORY TO THIS MAY AMPUTATE 1 (ONLY) CUNEIFORM CARTILAGE—DO ONE SIDE AT A TIME
TREAT REFLUX, ABX, STEROIDS, REASSURANCE AND TIME—INTERVENE WITH WT LOSS, POOR FEDING, CYANOSIS–OTHERWISE OBSERVE—NEVER HESITATE TO GET A 2ND OPINION!! AN ANNOYED PUT OUT PARENT IS BETTER THAN A DEVASTATED ONE.
NEW ENTITY DESCRIBE CALLED “STATE DEP LARYNGOMALACIA”—-(NEUROGENIC)—DEV STRIDOR WHEN ASLEEP—THE NEUROLOGICALLY IMPARED CHILD IS REALLY A DIFFERENT ANIMAL—DIFFUSE PHARYNGEAL HYPOTONIA
TRACHEOMALACIA/BRONCHOMALACIA
NOT RELATED TO LARYNGOMALACIA
ALWAYS RESOLVE IN THE FIRST YEAR OF LIFE
MORE COMMON IN DOWN SYNDROME
NEED 4.5/1 RATIO OF ARCH TO MEMBRANOUS TRACHEA (B.BENJAMIN)
EXP. STRIDOR
“DYING SPELLS”
MARKEDLY EXACERBATED BY URTI
HIGH INCIDENCE OF RECURRENT LOBAR PNEUMONIA (B PNEUMOTHORAX)
Dx: ENDOSCOPY–EXCLUSIVELY WITH APNEIC BRONCH
Rx: CPAP, TRACH—-AIRWAY STENTS HAVE BEEN DISAPPOINTING
ALWAYS TREAT FOR GERD
CONG LOBAR EMPHYSEMA
REALLY A DISTAL PULM MALACIA WHICH CAUSES EMPHYSEMATOUS EXPANSION OF THE AFFECTED LOBE (USUALLY LUL) AND THEN COMPRESSION OF THE OTHER NON-AFFECTED LOBES—-Rx = RESECTION OF THE AFFECTED LOBE
VALLECULAR OR SACCULAR CYST OF THE LARYNX (LARYNGOCELE)
OFTEN CAN DECOMRESS WITH A LARGE BORE NEEDLE AND SYRINGE
LARYNGEAL CYSTS = FLUID / LARYNGOCELES = AIR
BEST = RESECTION, BUT MARSUPULIZATION, AND DECOMPRESSION ARE OFTEN OK
LARYNGOCELE = DILATION OF THE SACCULE—- AIR FILLED AND COMMUNICATE WITH THE LUMEN
AN ENLARGEMENT/DILATION OF THE SACCULOUS OR APPENDIX FROM THE VESTIGE OF THE VENTRICLE OF MORGAGNE
OFTEN PRESENT WITH HOARSENESS, DYSPNEA, OR A NECK MASS
INFECTED = LARYNGOPYOCELE
SACCULAR CYSTS ARE MUCUS FILLED AND DO NOT COMMUNICATE WITH THE LUMEN
CAN BE EITHER EXTERNAL (MORE COMMON)-–EXTEND THROUGH THE THYROHYOID MEMBRANE (THROUGH THE INT BR OF THE SLN FORAMEN) OR
INTERNAL (ENTIRELY WITHIN THE LARYNX)OR
COMBINED “MIXED” INTERNAL AND EXTERNAL
EXTERNAL = NECK MASS WHICH ENLARGES NOT WITH VALSALVA(POS PULM PRESSURE AGAINST A CLOSED GLOTTIS) BUT WITH TRUMET PLAYERS REVERSE MUELLERS (SUPRAGLOTTIC)—- FURSTENBURG’S SIGN OF THE NECK
BRYCE SIGN = FARTING NOISE WHEN YOU DECOMPRESS IT MANUALLY—-CAN SOMETIMES GET THAT WITH A LARGE ZENKERS AS WELL
Dx = CT SCAN WITH CONTRANST
Rx = EXCISION BY LAT PHARYNGOTOMIES USUALLY NECESSARY
TVC NODULES (SCREAMERS) HYPERFUNCTIONAL AQUIRED NODULES
THE MOST COMMON AQUIRED LARYNGEAL PATHOLOGY
DISCRETE, WELL DEFINED
SYMMETRICAL—BETWEEN THE VOCAL PROCESS AND ANT COMMISURE
EPITHELIAL (CALLOUS LIKE) NON KERITINIZING SQUAMOUS EPITHELIUM
PRIOR TO CONSIDERING SURGERY WOULD NEED A MINIMUM OF 6 MONTHS INTENSIVE VOICE THERAPY AND ANTIREFLUX THERAPY–AND THEN GET A SECOND OPINION
PEH (PSUEDOEPITHELIOMATOUS HYPERPLASIA)—ASSOC WITH GRANULAR CELL TUMOR/ NECROTIZING SIALOMETAPLASIA—MIMICS SCCA. NOCYTOPATHIC CHANGES—MUST RULE OUT GRANULAR CELL TUMOR.
REINKES EDEMA (POLYPOID CORDITIS/LARYNGITIS/DEGENERATION, CHRONIC HYPERTROPHIC LARYNGITIS) AND TVC POLYPS—-SUBEPITHELIAL—REINKES EDEMA = A CHRONIC COLLECTION OF LOOSE GELATENOUS MATERIAL IN THE SUPERFICIAL LAYER OF THE L.P. —-BETWEEN THE NON KERITINIZING STRAT SQUAM EP OF THE TVC AND VOCAL LIGAMENT—-BOUNDED ANTERIORLY BY BROYLES LIG AND POSTERIORLY BY THE ARYTENOIDS
STRONG ASSOC WITH SMOKING, VOCAL ABUSE, AND GERD!!!
Rx—-ELIMINATE THE RISK FACTORS—-HIRANO’S METHOD OF INCISING THE SUP ASPECT OF THE TVC AND CREATING A MEDIALLY BASED FLAP—THE MYXOID GELATENOUS MATERIAL IS THEN SUCTIONED OUT THE THE FLAP REPLACED—-ANY EXCESS CAN BE TRIMMED
VOCAL PROCESS GRANULOMA (CONTACT ULCER)
GT ON POST 1/3 OF THE TVC / ARYTENOID SCLEROSIS ON CT SCAN
1) HYPERFUNCTIONAL—LOOK FOR SULCUS VOCALIS = ABNL FURROWING OF THE MEMBRANOUS TVC—LEADS TO FIBROSIS AND BOWING OF THE TVC
2) INTUBATIONAL
3) HYPERACIDIC (GERD)—-MOST COMMON AND PROBABLY AN CONTRIBUTING VARIABLE TO ALL
Rx: MONTHS OF CONSERVATIVE TREATMENT (BID PROTON PUMP INHIBITORS) , VOICE REST, SPEECH THERAPY, ABX, ANTACID, STEROIDS, ENDOSCOPIC REMOVAL (HIGH RECURRENCE RATE)—TALK OF BOTOX FOR REFRACTORY CASES
GERD/REFLUX LARYNGITIS— ”DELAHANTY’S SYNDROME”—POST GLOTTIC ERYTHEMA/ INFLAMMATION– DYSPHONIA PLICAE VENTRICULARIS—FVC BECOME HYPERTROPHIED—EDEMATOUS AND OVERRIDE THE TVC’S
BOWED TVC’S—-PSYCHOGENIC OR PRESBYLARYNX
ARYTENOID DISLOCATION—FROM A TRAUMATIC INTUBATION–THE ARYTENOID IS OBVIOUSLY ANTERIORLY DISPLACED
TVC (VAGAL) PARALYSIS—–THE SECOND MOST COMMON CONG LARYNGEAL ANOMALY
GET Hx, PE—PALPATE THE THYROID, ENDOSCOPY(PASSIVE MOBILITY), CT THE COURSE OF THE RLN VS CXR, LAT C-SPINE AND SKULL SERIES, BARIUM SWALLOW, THYROID SCAN, LP?, UA, ESR, CBC, GTT, MHATP, LYME TITERS?
CAVEATES:
OLIVER’S SIGN = TRACHEAL TUG SIGN–TRACHEA PULSATES
ORTNER’S SYNDROME= AORTIC ARCH ANEURYSM RESULTING IN HORSENESS
SOME BILAT INNERVATION OF THE INTERARYTENOIDEUS MUSCLE—OTHERWISE ALL IPSI
TEST SENSATION TO HELP LOCALIZE THE LESION
ALL MUSCLES -GLOSSUS- ARE INNERVATED BY CN 12 EXCEPT PALATOGLOSSUS (10)
ALL MUSCLES -PALATE- ARE INNERVATED BY CN 10 EXCEPT TENSOR VELI PALATINI
ALL MUSCLES TENSOR ARE INNERVATED BY CN 5 PERIOD (PORTIO MINOR, V3)
ALL INTRINSIC LARYNGEAL MUSCULATURE IS INNERVATED BY THE RLN EXCEPT FOR THE CRICOTHYROID (EXT. BR OF SLN)—THIS MUSCLE IS ALSO THE ONLY “INTRINSIC” MUSCLE EXTERNAL TO THE THYROID CARTILAGE—-SEE IT QUITE CLEARLY IN THYROID SURGERY
ALL INTRINSIC LARYNGEAL MUSCLES SERVE TO TIGHTEN OR ADDUCT THE CORDS EXCEPT THE POSTERIOR CRICOARYTENOID (PCA)
ALL INTRINSIC MUSCLES ARE PAIRED AND THUS INNERVATED IPSILATERALLY EXCEPT THE INTERARYTENOIDIUS—-BILAT INNERVATION VIA THE RLN—MAY SEE SOME ADDUCTION OF THE ARYTENOID IN A IPSI VAGAL PARALYSIS
THE ENTIRE SUPRAGLOTTIS IS AFFERENTLY INNERVATED BY THE INT BR OF THE SLN—RUNS JUST SUBMUCOSALLY IN THE APEX OF THE PIRIFORM SINUS—-CAN ANESTHETIZE IT HERE OR CAN INJECT THE REGION OF THE THYROHYOID MEMBRANE TRANSCUTANEOUSLY
THE INFRA GLOTTIC REGION IS AFFERENTED BY THE RLN—-THEY MEET AT GALEN’S ANASTOMOSIS
EXT LARYNGEAL MUSCLES DIVIDED INTO ELEVATORS (EXPIRATION) AND DEPRESSORS (INSP) BY THEIR INSERTION ON THE OBLIQUE LINE OF THE THYROID CARTILAGE—INNERVATED BY THE ANSA CERVICALIS (USUALLY BELOW THE CRICOID)
THE VAGUS NERVE EXITS THE JUGULAR FORAMEN WITH THE IJV, CN 9 AND 11
JUGULAR GANGLION IS USUALLY WITHIN THE CANAL—-GIVES OFF A MENINGEAL BRANCH WHICH SHOOTS BACK UP INTO THE CRANIUM
THEN GIVES OFF AN AURICULAR BRANCH (GSA)–ARNOLD’S NERVE
NEXT IS THE NODOSE GANGLION—ABOUT 1.5 CM UNTIL PHARYNGEAL BRANCH COMES OFF—-SVE–ALL PALATE MUSCLES EXCEPT TENSOR VELI PALATINI(V3)—-ALL PHARYNGEAL MUSCULATURE EXCEPT STYLOPHARYNGEUS(9)
SLN(4TH ARCH)—DIVIDES INTO THE INT AND EXT BR
INT BR SLN—ALL FROM NODOSE GANGLION
EXTEROCEPTIVE (GVA) FROM THE IPSI SUPRAGLOTTIC MUCOSA
PROPRIOCEPTIVE (GVA) FROM THE THYROEPIGLOTTIC JOINT AND THE CRICOTHYROID JOINT
GUSTATORY (SVA) FROM THE EPIGLOTTIS
EXT BR SLN
EXTEROCEPTIVE (GVA) FROM THE ANT SUBGLOTTIC MUCOSA
PROPRIOCEPTIVE (GVA) FROM THE CRICOTHYROID JOINT
MOTOR (SVE) TO THE OBLIQUE AND VERTICAL BELLIES OF THE CRICOTHYROID MUSCLE—TILTS THE THYROID ON THE CRICOID LIKE A VISOR
RLN (6TH ARCH)—-LOOPS AROUND THE AORTIC ARCH JUST PAST THE LIGAMENTUM ARTERIOSUM ON THE LEFT——LOOPS AROUND THE SUBCLAVIAN ARTERY ON THE RIGHT (ANOMALOUS R SUBCLAVIAN WHICH ORIGINATES FROM THE DECENDING AORTA INSTEAD OF THE INOMINANT(BRACHIOCEPHALIC TRUNK)—-FOLLOWS A RETROTRACHEAL (USUALLY RETROESOPHAGEAL) COURSE INTO THE R ARM)—CAN GIVE YOU BAYFORD’S SYNDROME OF INTERMITTENT DYSPHAGIA LUSORIA, WEIGHT LOSS AND A NON-RECURRENT R LARYNGEAL NERVE(0.6% INCIDENCE—SEEN IT)—CAN THEORETICALLY HAVE A LEFT NON-RECURRENT INF LARYNGEAL NERVE BUT YOU MUST HAVE BOTH SITUS INVERSUS AND A RETROESOPHAGEAL SUBCLAVIAN
EXTEROCEPTIVE (GVA) TO SUBGLOTTIC MUCOSA
ANTERTIOR (ADDUCTOR) BRANCH (SVE) TO MAJORITY OF INTRINSIC LARYNGEAL MUSCULATURE
POSTERIOR (ABDUCTOR) BRANCH (SVE) TO PCA—MORE SUSCEPTIBLE TO INURY—FEWER AND MORE TENUOUS THAN THE ADDUCTOR FIBERS
SEMON’S LAW—–VOICE WILL BE GOOD AND AIRWAY WILL BE MORE OF A PROBLEM THAN ASPIRATION—-”THE ACTION OF THE POSTERIOR BRANCH OF THE RLN (ABDUCTION) TO THE PCA WILL BE LOST FIRST AND RETURN LAST FOLLOWING INJURY”—-IN THYROID SURGERY HAVE SEMON’S LAW WORKING AGAINST YOU BUT THE ANT BRANCH MAY BE MORE AT RISK IN YOUR SURGICAL FIELD
SVE TO CRICOPHARYNGEUS ALONG WITH THE PHARYNGEAL PLEXUS
AORTIC BRANCH/PLEXUS
SVA TO CHEMORECEPTORS IN AORTIC BODY
CONG. VAGAL PARALYSIS
SECOND (OR THIRD) MOST COMMON CAUSE OF INFANT STRIDOR (2ND TO LARYNGOMALACIA—POSSIBLY THIRD TO SUBGLOTTIC STENOSIS)
UNILT 66%>BILAT 33%
UNILAT—SUBTLE Sx—-OFTEN MISSED—IN REALITY PROBABLY MUCH MORE PREVALENT—–NONE OF THE GENERAL SURGEONS EVER LOOK
NEED TO IMAGE ENTIRE COARSE OF RLN —–CONSIDER MOBIUS—-OFTEN IDIOPATHIC (6-8 WEEKS)
CAN BE IATROGENIC FROM REPAIR OF TEF
L>R—–SOME SOURCES SAY R>L (SHORTER, MORE EASILY STRETCHED
L—OFTEN ASSOC WITH CV OR PULM DEFECT
R—OFTEN ISOLATED FINDING
95% PERIPHERAL
WEAK OR MUFFLED CRY, STRIDOR (WORSE WITH AGITATION)
Rx: USUALLY NO TREATMENT–OBSERVE FOR AT LEAST 6 MONTHS—USUALLY RESOLVE IT
RARELY TRACH (<33%)
BILAT (>66%)
ALSO NEED TO IMAGE CNS—HIGH ASSOC. WITH CNS ABNL (HYDROCEPHALUS/ARNOLD CHIARI, MYELO/ENCEPHALO-MENINGOCELE, MR, BULBAR PAULSEY
USUALLY PRESENT WITH RESP DISTRESS
HIGH PITCHED INSP STRIDOR (WORSE WITH AGITATION)
NL CRY / NL VIOCE!—-LEADS TO DELAY IN Dx
ASPIRATION—RECURRENT PNEUMONIA
Rx: AFTER NEUROSURG VP SHUNTS THEM USUALLY RESOLVE PROBLEM WITHIN 2 WEEKS!!!—TRY TO WAIT FOR POSSIBLE SPONT. RECOVERY—-END UP TRACHING >66% OF TIME
ARYTENOIDECTOMY, ARYTENOPEXY, OR POST CRICOID SPLIT WITH COSTAL CARTILAGE GRAFTING—AT ABOUT AGE 2
POSSIBLE CORDOTOMY AFTER KASHIMA
NON-CONG. VAGAL PARALYSIS
40%–TRAUMA (5% THYROID SURGERY)
22%–NEOPLASTIC (PRIMARILY BRONCHOGENIC CA)—–PROBABLY NOW THE LEADING CAUSE
14-20%–IDIOPATHIC
5%–NEURO (CENTRAL)—POLIO, ALS
20%—OTHER/INFLAMMATORY
UNILAT (80%)
L 3 : 1 R
BILAT (20%)—PROBABLY PRIMARILY DUE TO THYROID SURGERY
VOCALIS MUSCLE PROBABLY HAS B INERVATION FROM BOTH THE RLN AND EBSLN
UMN—GET A HYPERTONIC (SPASTIC) PARALYSIS WITH THE TVC IN AN ABDUCTED POSITION
LMN—-FLACCID PARALYSIS WITH THE TVC IN A MORE MEDIAL POSITION
SLN ONLY:
RELATIVELY NL TVC POSITION
TVC BOWING (LOSS OF TENSION)–NO CRICOTHYROID TONE
LOSS OF UPPER SINGING REGISTERS (AMILITA GALIKERTZI)– -LOWERED VOICE—A DISASTER
POST COMMISURE ROTATED (CANTED) TO SIDE OF LESION—-SOME IPSI CAUDAD ROTATION
FAILURE OF EPIGLOTTIS TO MOVE ANT
MUCOSAL HYPESTHESIA
POOLING OF SECRETIONS
REVERSAL OF GUTTMAN’S TEST—NORMALLY THE VOICE LOWERS WITH ANT PRESSURE OPN THE THYROID CARTILAGE AND RAISES WITH LAT PRESSURE
CAN SUTURE THE THYROID CARTILAGE TO THE CRICOID TO COMPENSATE FOR THE LACK OF CRICOTHYROID ACTIVITY
RLN ONLY:—–MAY BE DUE TO AN ISCHEMIC NEUROPRAXIA (POST GETA)ON THE ANT. BR OF THE RLN
STRAIGHT (NOT-BOWED) TVC—-PASSIVE TENSION ON TVC FROM CRICOTHYROID (SLN)
TVC ATROPHY
BILAT—ANT AND INTERARYTENOID GAP
UNILAT—CORD ININTERMEDIATE–THEN– PARAMEDIAN POSITION WITH ANT. GLOTTIC GAP—GET REINNERVATION OF INTERARYENOID MUSCLE–ANT GLOTTIC GAP ONLY
SEMON’S LAW—THE ACTION OF THE PCA (ABDUCTION) IS LOST 1ST AND RETURNS LAST IN RLN INJURY
RLN & SLN
CORD(S) IN IN INTERMEDIATE POSITION
VOCAL CORD ATROPHY AND BOWING
PHONOSURGERY—-BRUNING (1911)—PARAFFIN INJ, PAYR (1915)–POST LARYNGOFISSURE, ARNOLD (1952)—-TEFLON, ISSHIKI (1975)—-TYPE I THYROPLASTY (ALLOPLASTIC-SILASTIC- BLOCK)
IF EXPECTED RETURN–—DO GELFOAM INJECTION—–LAT TO THE MUSCLE—AS CLOSE TO THE INTERNAL THYROID ALA AS POSSIBLE—REGRESSES IN ABOUT 6 WEEKS, CAN ALSO DO TYPE I THYROPLASTY—–BOTH REVERSIBLE
IF NO CHANCE OF RETURN—-TEFLON INJECTION IS A POSSIBILITY, FAT, GELFOAM OR COLLAGEN MAY BE LESS PERMANENT—
TYPE I THYROPLASTY -REVERSIBLE
THE NIGHT BEFORE CUT SOME SILASTIC BLOCKS
MAKE A TRANSVERSE INCISION OVER THE IPSI ALA—RAISE A SUBPLATYSMAL FLAP TO THE HYOID AND INF TO THE CRICOID
DEFINE THE MIDLINE AT THE LARYNGEAL PROMINENCE—-CUT DOWN THROUGH THE PERISOTEUM WITH A 15 BLADE AND JUST RAISE EVERYTHING OFF THE THYROID CARTILAGE MEDIAL TO LATERAL
MARK MIDWAY DOWN ANTERIORLY—THIS WILL BE EVEN WITH THE SUP WINDOW
MARK YOUR WINDOW—KEEP AT LEAST 3-4 MM INFERIORLY—CUT OR DRILL IT OUT—-LEAVE THE INTERNAL PERICHONDRIUM INTACT—RAISE THIS UP WITH A COTTLE—THEN CUT THE SUP, INF AND POST ASPECTS OF IT
MEASURE—PUT YOUR BLOCKS IN
CLOSE OVER A DRAIN
GIVE ABX AND STEROID—WATCH OVERNIGHT
MONTGOMERY SYSTEM HAS PROVEN SAFE EFFECTIVE AND RELIABLE IN MY HANDS
ARYTENOID ADDUCTION—-THIS IS IRREVERSIBLE (DO TO ANKYLOSSIS OF THE JOINT—ALSO HIGH RISKTOTHE RLN IN THIS PROCEDURE— BASICALLY TEATHER (SUTURE) THE MUSCULAR PROCESS OF THE ARYTENOID AND PULL IT LATERALLY TO ROTATE THE VOCAL PROCESS OUT INTO THE POST GLOTTIC MIDLIN THUS TIGHTENING THE TVC AND ELIMINATING THE POST GLOTTIC CHINK
LIPOINJECTION LARYNGOPLASTY
CAN BE A FAIRLY PERMANENT—EASY PROCEDURE
CAN DO UNDER LOCAL WITH MAC IF YOU CHOOSE—-PROBABLY EASIER TO JUST USE A SMALL ORAL ETT
HARVEST ABDOMINAL FAT—–NO SALINE, NO EPI IN YOUR LIDOCAINE
DICE IT UP INTO 1-3MM PEICES (OBTAIN 3-4CC)
LOAD IT INTO A BRUENING’S SYRINGE
INJECT INTO THE MID MEMBRANOUS CORD (JUNCTION OF ANT AND MID 1/3) AND OVER VOCAL PROCESS OF ARYTENOID (JUNCTION OF POST AND MID 1/3) DEEP IN THE VENTRICLE INTO THE THYROARYTENOID MUSCLE
OBTAIN AT LEAST A 50% OVER CORRECTION—CORD SHOULD APPEAR SIGNIFICANTLY CONVEX
CAN ALSO DO ANSA TO RLN ANASTOMOSIS TO TRY TO GET SOME TONE IN THE LARYNX
GLOTTIC INSUFICIENCY— TYPE II THYROPLASTY—-ANT THYROID ALA SPLIT—-RAISES VOICE, LASER CORDOTOMY, ARYTENOIDECTOMY—ISHIKI ASPOUSES FOR SPASMOTIC DYSPHONIA
LOWER VOICE—TYPE III THYROPLASTY—SHORTEN LAT THYROID ALA
RAISE VOICE—TYPE IV THYROPLASTY—SUTURE SHORTEN THE CRICOTHRYROIDMEMBRANE
CONG. LARYNGEAL (GLOTTIC) WEBS
? MOST LIFE THREATENING ANOMALY?
75% GLOTTIC
USUALLY ANT
APHONIC OR HIGH PITCHED CRY OR SQUEAK
MAY REQUIRE AN IMMEDIATE TRACH
Rx: LARYNGOFISSURE WITH KEEL (MAY GET AWAY MANAGING ENDOSCOPICALLY IF WEB IS THIN)
TEF
FEEDING PROBLEMS AND CYANOSIS
RECURRENT PNEUMONIA-—–USUALLY LEFT SIDED AS THE TRACHEA CROSSES THE L MAINSTEM
COUGHS WITH FEEDING
ASSOC. WITH MATERNAL POLYHYDRAMNIOS
87%—ESOPHAGEAL ATRESIA WITH DISTAL TEF
Dx: BARIUM SWALLOW/ —-ALTHOUGH IT CAN OTEN BE MISSED BY CONTRAST STUDY—MUST DO ENDOSCOPY
PLC—PARSONS PAPER
SIMILAR SX TO TEF—-ASSOC WITH ASPIRATION
TYPES I – IV BASED ON DEPTH (MAY EXTEND DOWN TO CARINA) (TYPE II GOES DOWN TO THE CRICOID)
CAN CLOSE BY EXT. APPROACH, LARYNGOFISSURE, OR ENDOSCOPICALLY
ASSOC WITH SUBGLOTTIC CRICOID STENOSIS
BEST TO DX WITH SUSPENSION LARYNGOSCOPY AND A 90 DEGREE PROBE
BIFID EPIGLOTTIS
RARE—ASSOC WITH OTHER MIDLINE DEFECTS (HYPOSPADIUS, PLC, HYPOPITUITARISM)
SUBGLOTTIC HEMANGIOMA
HEMANGIOMA IS MOST COMMON PEDIATRIC NEOPLASM—50% WILL HAVE AN ASSOC CUTANEOUS LESION
USUALLY PRESENT BY 3 MONTHS OF AGE—MOST PRESENT AT BIRTH
BIPHASIC STRIDOR — WORSE WITH CRYING (VALSALVA–VENOUS CONGESTION)
GROWTH AND INVOLUTIONAL PHASES
MOST RESOLVE BY AGE 2
FEMALE 2:1
PRIMARILY LEFT POST/LAT QUADRANT
CAPILLARY>CAVERNOUS
Rx: BEST = OBS, CO2 LASER WITH POST OP INTUBATION, IV STEROIDS–DEXAMETHASONE SODIUM PHOSPHATE 1 MG/KG/DAY FOR A COUPLE OF WEEKS FOLLOWED WITH A PO PREDNISONE TAPER
HOLINGER ABLE TO AVOID TRACH MOST OF THE TIME WITH PO STEROIDS, ENDOSCOPIC LASER, STEROID INTRALESIONALINJECTION, AND POST PROCEDURE INTUBATION (FOR ABOUT 2 DAYS)
POSSIBLY TRACH AND OPEN RESECTION
SUBGLOTTIC CYST
USALLY ENDOSCOPIC MARSUPULIZATION AND IV STERIODS AND ABX
LASER IN THE AIRWAY
LASER FOIL WRAP YOUR ETT OR TRACH TUBE—–USUALLY IF YOU HAVE A TRACH JUST REPLACE IT WITH A WRAPPED ETT—–SET YOUR KTP (PENETRATES 0.9MM AT A WAVELENGTH OF 532 NM) ON 40 WATTS OR LESS AND PULSE IT (LESS THAN 1 SECOND)—-(MORE THAN THIS MAY GIVE YOU A POPCORN EFFECT OF DEEP THERMAL DAMAGE)—USE A SMALL FIBER (.4 MM)—-USE THE LEAST FLAMMABLE AND MOST STABLE GAS (NO2) Y0U CAN TO AVOID AIRWAY FIRES
NEVER LASER MORE THAN 1/3 OF THE SURFACE AREA OF THE LUMEN OR CICATRICIAL SCARRING MAY BE A PROBLEM
SUBGLOTTIC STENOSIS
2ND OR 3RD MOST COMMON CAUSE OF INFANT STRIDOR—”THERE IS NO SUCH THING AS CROUP UNDER THE AGE OF 1″
MOST COMMON IN WHITE MALES
LARYNGEAL CLEFTS ARE ALMOST ALWAYS ASSOC WITH CRICOID CARTILAGE STENOSIS
DIVIDED INTO CONGENTITAL AND AQUIRED
CONGENITAL DIVIDED INTO CIRCUMFIRENTIAL MEMBRANOUS (FAILURE OF CANALIZATION) AND CARTILAGENOUS (LATERAL SHELVES)
AQUIRED (2-8% POST LONG TERM INTUBATION–MOST COMMON ETIOLOGY— -HIGH ASSOCIATION WITH GERD, BPD, AND REACTIVE AIRWAY DISEASE)
OFTEN ASSOC WITH CLEFT PALATE, IMPERFORATE ANUS, AND TEF
USUALLY ABOUT 2-3 MM BELOW THE TVC’S
INITIALLY INSP—-THEN PROGRESSIVE BIPHASIC STRIDOR
USUALLY PRESENT EARLY IN LIFE—FIRST WEEKS TO MONTHS—-OFTEN AS RECURRENT/EPISODIC CROUP
CONSIDERED STENOTIC IF LESS THAN 3.5- 4 MM DIAMETER IN ANY DIRECTION—–WITH TODAYS PREMIES THIS MAY NEED TO BE REDEFINED
CONG.—MOST WILL RESOLVE SPONT WITH CRICOID GROWTH (45% REQUIRE A TRACH?)
AQUIRED–3% LONG TERM INTUBATION—MOST REQUIRE REPAIR(95% REQUIERE A TRACH)
<50% REDUCTION IN CROSS SECTIONAL AREA DO WELL
GRADE I = 50-70%–CAN USUALLY BE FOLLOWED, GRADE II = 70-90%, GRADE III = 90-99%–BUT WITH LUMEN, GRADE IV = NO LUMEN
USE ETT SIZE TO ASSESS GRADE—-GET A LEAK BETWEEN 5 AND 30 CM H2O
MEDICAL Hx, PFT’S(DELAY REPAIR UNTIL CHILD NOT VENT DEP, CONSIDER FUTURE NEED FOR ANESTHETIC, WORK UP AND TREAT GERD, CONSIDER T & A, CONSIDER HOME CARE ENVIRONMENT, COMPLETE ENDOSCOPIC EXAM TO ASSURE NO SECOND LESION—-R/O GERD, NEURO PROBLEMS, HIGHOUTPUT CARDIAC ABNL WITH RESULTANT DYSPNEA
Rx: GRADE I MAY BE AMENABLE TO ENDOSCOPIC MANAGEMENT
SURGERY MAY LEAD TO A WORSENING OF THE STENOSIS
MUST HAVE RESOLVED ANY LOWER AIRWAY COMPROMISE—ALSO STENOSIS MUST BE “MATURE”
STEPS: ASSESSMENT, SURGICAL CORRECTION, STABILIZATION, HEALING, DECANNULATION
ANT CRICOID SPLIT = ANT LARYNGOTRACHEAL DECOMPRESSION—-REALLY RESERVED FOR PREMATURE INFANTS WHO FAIL EXTUBATION—REALLY JUST ALLOWS EDEMA TO RESOLVE—-TRY TO WAIT UNTIL CHILD > 1500 GM—CUT ANT INF THYROID, CRICOID, AND 1ST 2 TRACHEAL ARCHES—-CONSIDER A CENTRAO HYOID INTERPOSITION GRAFT—PROBABLY LEAVE INTUBATED FOR 1-2 WEEKS WITH A PRETTY GOOD SIZED ETT TO STENT THINGS
LTR (LARYNGOTRACHEOPLASTY)—-TODAY ATTEMPT TO DO SINGLE STAGE SURGERY(REMOVE TRACH) FOR ALL GRADE I AND II LESIONS—OFTEN EXTUBATE IN UNIT AFTER LEAK AT 25 MM H2O—-MAY DO ANT AND POST GRAFTING +/- LATERAL GRAFTS—-COVER WITH STEROIDS AND ABX AND ANTIREFLUX MEDS
COMPLETE TRACHEAL RINGS/TRACHEAL STENOSIS
SEGMENTAL, LONG SEGEMENT, OR FUNNEL TYPES
CARINAL INVOLVEMNET PORTENDS POOR Px
Rx = OPEN TRACHEOPLASTY WITH HEART LUNG MACHINE
TRACHEAL TRANSPLANT WORKS WELL
TRACHEAL REPAIR/RESECTION
3 RINGS REMOVAL = MAX PRIOR TO RELEASING PROCEDURES
?NEED FOR RLN DISSECTION
RULE OF 4’S—-4MM UP, 4MM IN(BETWEEN SUTURES), WITH 4-0 VICRYL
VASCULAR ANOMALIES—TRACHEAL OR MAINSTEM COMPRESSION
CAN ALL CAUSE: REFLEX APNEA, REFLEX COUGH, EXP STRIDOR, DYSPHAGIA, RECURRENT PNEUMONIA
#1 AORTIC ARCH ANOMALY—TRACHEAL COMPRESSION
DOUBLE AORTIC ARCH (PERSISTENCE OF BOTH 4TH ARCH VESSELS) OR R AORTIC ARCH = THE MOST COMMON VASCULAR ANOMALY CAUSING STRIDOR IN THE NEONATE—BIPHASIC STRIDOR, DYSPHAGIA, AND CYANOSIS IN THE NEONATE
Rx: LIGATE THE NON-DOMINANT AORTIC ARCH—-ANT FROM THE RIGHT WHEREAS THE POST (DOMINANT) FROM THE LEFT
#2 INNOMINATE (BCT) ARTERY COMPRESSION
COMRESSES ANT WALL OF DISTAL TRACHEA
IS NOT ABBERANT—-NL ANATOMY HAS BCT AND L COMMON CAROTID LEAVING AORTIC ARCH AN TO THE TRACHEA FROM THE 7TH SEGMENTAL MESENCHYME
DIAGNOSTIC MANUEVER IS RIDGIC BRONCH COMPRESSION AND CORRELATION WITH RADIAL PULSE—-Rx INVOLVES OBSERVATION VS SUSPENSION TO THE ANT STERNUM
#3 ABERRANT SUBCLAVIAN ARTERY
CAN BE EITHER RETRO-TRACHEAL OR RETRO-ESOPHAGEAL
DYSPHAGIA LUSORIA (BAYFORD’S SYNDROME) = THE MOST COMMON MAJOR VASCULAR ANOMALY COMPRESSING THE UPPER AERODIGESTIVE TRACT—ASSOC WITH NON-RECURRENT R LARYNGEAL NERVE—COMES RIGHT OFF THE VAGUS
QUITE MINOR—CAN MAKE IT TO ADULTHOOD BEFORE IT BOTHERS THEM—ALWAYS IMPROVES WITH GROWTH WHEN THEY ARE ASYMPTOMATIC
#4 PULM ARTERY SLING
COMPRESSION OF TRACHEA AND R MAINSTEM BRONCHUS
Dx: MRI, BARIUM ESOPHAGRAM, ENDOSCOPY
Rx: PRIMARILY CONSERVATIVE, PARTIAL THYMECTOMY, VARIOUS PEXY OR DIVISION PROCEDURES
EXTRAPULMONARY CAUSES OF NEONATAL RESP DISTRESS
PHRENIC NERVE PARALYSIS, CONG. HEART Dz, ANEMIA, POLYCYTHEMIA, METABOLIC DISORDERS, CNS DISORDERS, ABD. MASSES OR DISTENTION
FOREIGN BODIES
TOTAL UPPER AIRWAY OBST—-APHONIA, NOCOUGH, NO CHOKING, UNIVERSAL “I’M CHOKING SIGN”—-HEIMLICH MANEUVER—FINGER SWEEP—-DIAPHRGMATIC THRUSTS—CRICOTHYROIDOTOMY
LARYNGEAL F.B. ASSOC WITH THE HIGHEST MORTALITY!
PEDIATRIC F.B. (USUALLY 6 MONTHS TO LATE CHILDHOOD)
Hx: ABRUPT ONSET PE: CHOKING, STRIDOR, WHEEZING— USE DOUBLE HEADED STETHOSCOPE—HIGH KV RADIOGRAPHS(XERORADIOGRAPHY—SOMETIMES PICK UP SOME RADIOLUSCENT F.B.’S), INSP. AND EXP. FILMS, FLOUROSCOPY—–GO TO RIDGID OR FLEXIBLE ENDOSCOPY
COINS TEND TO STICK AT THE CRICOPHARYNGEUS—LIE IN CORONAL PLANE IN THE HYPOPHARYNX AND IN THE SAGITAL PLANE IN THE LARYNX
DISK BATTERIES CAN QUICKLY LEAD TO AN ALKALINE BURN
BALLOONS ARE FREQUENLY DEADLY –THE GREATEST RISK FOR ASPHIXIATION
MACROGLOSSIA–AMYLOIDOSIS (BEWARE OF ECTOPY), DS
GLOSSOPTOSIS—-PIERRE ROBIN SEQUENCE—ANT GLOSSAL SUSPENSION, LIP ADHESION, NASAL TRUMPET, —–MAY NEED A TRACH—–GET AN AUDIO AND AN OPTHO CONSULT AS IT COULD BE A PART OF AUTO D STICKLER SYNDROME
FIX THE PALATE ONLY AFTER THE MANDIBULAR GROWTH HAS RELEIVED THE AIRWAY OBST
COUGH—–A SYMPTOM —NOT A Dx—- 50% ASSOC WITH LPR (RELFUX)
COUGH RECEPTORS OF THE SLN AND RLN CONCENTRATED AT GALENS ANASTOMOSIS
CARINA IS THE MOST SENSITIVE SPOT FOR A COUGH REFLEX
MAY VOLUNTARILY SUPPRESS YOUR COUGH
4 PHASES OF COUGH—-INSP—-CONTRACTIVE—-COMRESSIVE “TUSSIVE SQUEEZE”—-EXPLOSIVE “BECHIC BLAST” (CHEVELIER JACKSON)—MAY REACH THE SPEED OF SOUND
SMALLER AIRWAYS CORRELATE WITH BRONCHOCONSTRICTION
ETIOLOGY AND TREATMENT
PND—(40%)–ABX, ATROVENT NASAL SPRAY, STEROID NASAL SPRAY (RHINOCORT/NASOCORT), HTSI, ANTIHISTAMINE (P.O. OR NASAL SPRAY), NASAL TILADE
ASTHMA—(COUGH VARIANT ASTHMA)–25%—EXCERCISE, NOCTURNAL, OR COLD EXPOSURE COUGH)—-TILADE, ALBUTEROL, MDI (STEROIDS)—CONSIDER METHACHOLINE OR HISTAMINE PROVOCATION TEST
GERD/REFLUX--20%–”THE Dx OF THE 90’S”
OFTEN POST PRANDIAL OR NOCTURNAL NON PRODUCTIVE COUGH–GLOBUS PHARYNGEUS, STRESS, HORSENESS, CHRONIC THROAT CLEARING–SX WORSE IN THE AM–OTALGIA, CERVICAL ODYNOPHAGIA, NUT CRACKER ESOPHAGUS—MOST DO NOT HAVE PYROSIS
PE—-OVERWEIGHT, SMOKERS/DRINKER–ANTIDEPRESSANTS, CAFFEINE, ETOH, B BLOCKERS
CISAPRIDE/REGLAN, H-2 BLOCKER, PROTON PUMP INHIBITOR=BEST
ROUTINE PRECAUTIONS (HOB UP 6-8 INCHES), WT LOSS, D/C CAFFFEINE, D/C ETOH, D/C NICOTINE DO NOT EAT OR DRINK AFTER 1900
Dx—-Hx—ENDOSCOPY—COBBLESTONING–Bx THE ESOPHAGUS FOR INFLAMMATORY OR METAPLASTIC CHANGES—BRONCHOALVEOLAR LAVAGE–LIPID LAYDEN MACROPHAGES (3 DAY ½ LIFE)—-PH PROBE, BARIUM STUDY, MANOMETRY
DL—POST GLOTTIC LARYNGITIS, DIFFUSE NONEYTHEMATOUS LARYNGEAL EDEMA, DIFFUSE ERYTHEMA, OR DISCRETE GRANULOMA
ASSOC WITH SIDS, LARYNGOMALACIA,GLOBOUS, LARYNGOSPASM, REACTIVE AIRWAY Dz, ASPIRATION PNEUMONIA, LARYNGOTRACHEAL STENOSIS, ECT….
CHRONIC BRONCHITIS—-5%–ABX–REMOVE IRRITANT—SMOKERS–COPIOUS SPUTUM—ESPECIALLY IN THE A.M.
QUESTION PARENTS ABOUT 2ND HAND SMOKE
ALLERGY-— POLLUTION—–OFTEN A SEASONAL OR OTHER PATTERN—AVOIDNCE, PHARMICOTHERAPY, IMMUNOTHERAPY
INFXN—MACROLIDE (ATYPICAL, ARCHIBACTERIA(CHLAMYDIA RO MYCOPLASMA)—VIRAL “100 DAY” COUGH, PERTUSSIS=WHOOPING COUGH)—- TB-MOST COMMON IN THE 3RD WORLD
MEDS-–ACE INHIBITORS, BETA BLOCKERS
ORGANIC ANOMALY—EXAMINE PT–INFANTS—-LARYNGOMALACIA- –FOREIGN BODY—-COUGH WHEN THEY EAT — THINK–TEF, PLC, AORTIC ARCH ANOMALY–THINK OF CF—OTOLOGIC IRRITANT, DIAPHRAGMATIC IRRITATION, SARCOID (SILENT ON ASCULTATION)
MEDICAL Dz-—CF, NEOPLASM, HEART FAILURE—-RHEUMATOID ARTHRITIS AND ARYTENOID JOINT ABNL (TRY NSAIDS)
PHYSCOGENIC COUGH-–THE ONLY ONE WHICH IMPROVES AT NIGHT—”HABIT COUGH”—-OFTEN SOUNDS LIKE A CANADIAN GOOSE—MY OFTEN BE A CONVERSION RXN FROM STRESS OR PHOBIA
Dx/Rx—-GET A CXR EARLY—CBC, PPD, ICAP, TRIAL OF PROTON PUMP INHIBITOR
CHILDREN MAY HAVE PERSISTENT COUGH FOR WEEKS AFTER A URTI
ADULTS—-TREAT PND AGGRESSIVELY FOR 1-2 WEEKS—–THEN IF STILL PRESENT
TREAT GERD AGGRESSIVELY FOR AT LEAST 2 WEEKS——THEN IF STILL PRESENT
GET PFT’S AND METHACHOLINE CHALLENGE FOR COUGH VARIANT ASTHMA AND GET CT OF SINUSES
FINALLY DO ENDOSCOPY
SYMPTOMATIC TREATMENT—-CODEINE, HYDROCODONE ELIXER, TESSALON PERLES (BENZOATE), VANCERIL, TILADE
THINK OF CHRONIC HORSENESS THE SAME WAY—BUT ALSO CONSIDER HYPOTHYROIDISM