 Utilizing Flovent 220 with a modified baby nipple in the nose might be a significant adjuvant tool for refractory polyp patients. In talking with other allergists and sinus physicians I am always excited to steal from others and add to my own bag of tricks.
Utilizing Flovent 220 with a modified baby nipple in the nose might be a significant adjuvant tool for refractory polyp patients. In talking with other allergists and sinus physicians I am always excited to steal from others and add to my own bag of tricks.
Fatal Reactions with SCIT
The biggest fear in allergy shots is the severe, or even fatal, reaction. Each year 3-4 people die from a severe allergic reaction to allergy shots. The biggest risk seems to be poorly controlled asthma. Epinephrine given immediately is the most important intervention. The reaction can happen up to 30 minutes after the shot, however, the vast majority happen within 15 minutes. If an epinephrine injection is given, the patient should be ready to need another treatment. Biphasic reactions are common and can happen hours later. Drawing a tryptase level and instituting steroids seems appropriate. Interestingly, large local reactions do not clearly predict systemic reactions. However, they may still require a dose reduction.
Pertussis (Whooping Cough)
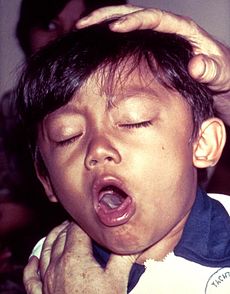 Pertussis, also known as whooping cough, is a highly contagious respiratory disease. It is caused by the bacterium Bordetella pertussis.
Pertussis, also known as whooping cough, is a highly contagious respiratory disease. It is caused by the bacterium Bordetella pertussis.
Pertussis is known for uncontrollable, violent coughing which often makes it hard to breathe. After fits of many coughs, someone with pertussis often needs to take deep breathes which result in a “whooping” sound. Pertussis most commonly affects infants and young children and can be fatal, especially in babies less than 1 year of age. In adults it often manifests as the “100 days cough.”
The classic symptoms of pertussis are a paroxysmal cough, inspiratory whoop, and fainting and/or vomiting after coughing.[5] The cough from pertussis has been documented to cause subconjunctival hemorrhages, rib fractures, urinary incontinence, hernias, post-cough fainting, and vertebral artery dissection.[5] Violent coughing can cause the pleura to rupture, leading to a pneumothorax. If there is vomiting after a coughing spell or an inspiratory whooping sound on coughing, the likelihood almost doubles that the illness is pertussis. On the other hand, the absence of a paroxysmal cough or posttussive emesis makes it almost half as likely.[5]
The incubation period is typically seven to ten days with a range of four to 21 days and rarely may be as long as 42 days,[6] after which there are usually mild respiratory symptoms, mild coughing, sneezing, or runny nose. This is known as the catarrhal stage. After one to two weeks, the coughing classically develops into uncontrollable fits, each with five to ten forceful coughs, followed by a high-pitched “whoop” sound in younger children, or a gasping sound in older children, as the patient struggles to breathe in afterwards (paroxysmal stage).
Fits can occur on their own or can be triggered by yawning, stretching, laughing, eating or yelling; they usually occur in groups, with multiple episodes every hour around the clock. This stage usually lasts two to eight weeks, or sometimes longer. A gradual transition then occurs to the convalescent stage, which usually lasts one to two weeks. This stage is marked by a decrease in paroxysms of coughing, both in frequency and severity, and a cessation of vomiting. A tendency to produce the “whooping” sound after coughing may remain for a considerable period after the disease itself has cleared up.
The best way to protect against pertussis is immunization. The immunization is primarily given as the DPT vaccine and is generally considered safe and cost effective. Treatment with a macrolide or Bactrim is first line. Diagnosis is made with a nasopharyngeal swab cultured in Bordet-Gengou medium.
Chronic Cough
 The Chronic Cough is a very common complaint in both our adult and pediatric patients. History and Physical exam are paramount and ruling out a worrisome etiology is our initial objective. After this is accomplished the etiology is almost always multifactorial. LPR, Cough variant asthma, PND associated with Allergic rhinitis, and Infectious etiologies are highest on our differential.
The Chronic Cough is a very common complaint in both our adult and pediatric patients. History and Physical exam are paramount and ruling out a worrisome etiology is our initial objective. After this is accomplished the etiology is almost always multifactorial. LPR, Cough variant asthma, PND associated with Allergic rhinitis, and Infectious etiologies are highest on our differential.
Delphian Node
![delphian node[6]](http://www.midwestsinus.com/wp-content/uploads/2014/01/delphian-node6.png) The Delphian (DL) node, also called the prelaryngeal or cricothyroid node, is a lymph node located on the fascia above the cricothyroid membrane. The DL node receives afferent lymphatic drainage from the larynx (supraglottis and subglottis via the anterior commissure) and the thyroid gland (upper and anterior portions of both lobes and isthmus). The DL node has two main efferent lymphatic drainage routes: one flows toward the pretracheal (sub-DL), mediastinal, supraclavicular nodes and the other to the paratracheal and lower jugular (Level IV) nodes (Fig. 1). The expression ‘Delphian’ was first used by R. Randall, at the time a medical student at Harvard, because a metastasis to the DL node may predict the prognostic outcome of laryngeal and thyroid cancers, in the same way the prophecy of Apollo at temple of Delphi foretold the future in ancient Greece. The Oracle of Delphi in this case would make the dire prediction that death from Squamous Cell or Thyroid Cell carcinoma is pending.
The Delphian (DL) node, also called the prelaryngeal or cricothyroid node, is a lymph node located on the fascia above the cricothyroid membrane. The DL node receives afferent lymphatic drainage from the larynx (supraglottis and subglottis via the anterior commissure) and the thyroid gland (upper and anterior portions of both lobes and isthmus). The DL node has two main efferent lymphatic drainage routes: one flows toward the pretracheal (sub-DL), mediastinal, supraclavicular nodes and the other to the paratracheal and lower jugular (Level IV) nodes (Fig. 1). The expression ‘Delphian’ was first used by R. Randall, at the time a medical student at Harvard, because a metastasis to the DL node may predict the prognostic outcome of laryngeal and thyroid cancers, in the same way the prophecy of Apollo at temple of Delphi foretold the future in ancient Greece. The Oracle of Delphi in this case would make the dire prediction that death from Squamous Cell or Thyroid Cell carcinoma is pending.
Oral Immunotherapy is finally here
 For much of her adult life, Shirley Hickey received two injections a week in an effort to tame severe allergies that caused frequent sore throats and sinus infections. Now she uses a less painful method.
For much of her adult life, Shirley Hickey received two injections a week in an effort to tame severe allergies that caused frequent sore throats and sinus infections. Now she uses a less painful method.
“One drop under the tongue every morning, and that’s it,” said Ms. Hickey, 65, who lives in Beaver Falls, Pa. She is free of symptoms and sinus infections from her allergies to ragweed and tree pollens, she said.
Injections have been used to treat allergies from inhaled substances — often known as hay fever — for 100 years, and the basic formula has changed little. But an alternative is now emerging — liquids or tablets placed under the tongue.
Both Merck and Stallergenes, a French company, are seeking marketing approval for tablets to treat grass pollen allergies. An advisory committee to the Food and Drug Administration will discuss the drugs next week.
The drugs are already available in Europe. If they are approved in the United States, they could make this type of therapy more broadly available, by allowing people to treat themselves at home rather than going for frequent shots. Children, who tend not to like needles, might also find such treatment more acceptable. Approval would also deliver some extra credibility to this type of therapy, which aims to fundamentally alter the immune system.
“It’s hugely important,” said Dr. Linda S. Cox, president of the American Academy of Allergy, Asthma and Immunology.
But there are drawbacks. The shots can be tailored to match the patient’s allergies while the liquid drops and tablets are standardized.
An estimated 30 million to 60 million Americans, including up to 40 percent of children and 10 to 30 percent of adults, suffer nasal congestion, runny nose, sneezing, itchy eyes or other symptoms from allergies to something they inhale.
The typical treatments are antihistamines or nasal steroids. But those drugs merely alleviate symptoms.
Immunotherapy, as allergy shots and under-the-tongue treatments are called, involves giving controlled doses of the allergen to teach the immune system to tolerate it. That can lead to longer-lasting relief.
Some studies have shown that three years of immunotherapy provides substantial relief for two years after treatment is stopped, in some cases for longer. Some studies also suggest that immunotherapy can reduce the risk of developing asthma.
But only a small percentage of people with respiratory allergies get the shots.
One reason is that people have to visit the doctor for shots at frequencies ranging from twice a week to once a month for several years. Another is that immunotherapy, while now broadly accepted as studies have accumulated, has had its doubters.
“Allergists always had a bad rap,” said Dr. David P. Skoner, chief of allergy, asthma and immunology at Allegheny Health Network in Pittsburgh. “We were called quacks and shot doctors. The reason was the science wasn’t there.”
The allergen extracts used for the shots are approved by the F.D.A. on the basis of their safety, purity and potency. But because immunotherapy has been around for so long, extracts generally do not go through clinical trials to prove they can actually help tame allergies.
Merck and Stallergenes, by contrast, have done controlled clinical trials and are seeking approval on the same basis as any other drug. That could enhance the credibility of the treatments.
In Merck’s biggest trial, involving 1,500 adults and children who are allergic to Timothy grass, those who took the tablets had a 20 percent reduction in symptoms during one allergy season compared with those who received a placebo. They also used antihistamines or other symptom-relieving drugs less often. Stallergenes’ results were in the same ballpark.
Still, not all allergists will welcome the tablets. That is because they make money giving shots, while the tablets would be prescribed like other pills.
“The allergists in the United States are frightened by this, concerned about it, a little paranoid about it,” said Dr. Skoner, who is also a professor at Temple University and West Virginia University and a consultant to Merck.
The sublingual tablets are kept under the tongue for about a minute, allowing them to dissolve, pass through the mucous membranes and be taken up by immune system cells.
Stallergenes’ product, called Oralair, contains extracts from five grass pollens. If approved, it would be marketed by Greer Laboratories, an allergen extract manufacturer based in North Carolina.
Merck’s product, which the company proposes to call Grastek, contains extract only from Timothy grass. Merck licensed its product from a Danish company, ALK-Abello, which sells it in Europe under the name Grazax.
Oralair is meant to be taken for about six months a year, starting four months before the grass pollen season and extending through the season. Merck’s drug is meant to be taken year-round.
Merck has also applied for approval of a tablet, also licensed from ALK-Abello, to treat ragweed allergy. Greer is developing a liquid sublingual product for ragweed. Sublingual therapy for dust mite allergy might come after that.
Grazax and Oralair have been available in Europe for several years. A variety of factors, including the time needed to do American clinical trials, explain why it has taken so long for the drugs to reach the United States.
Some American doctors have not waited. A survey in 2011 found that 11 percent of allergists were using the extracts approved for injection as off-label sublingual treatments. That is the treatment Ms. Hickey is using.
Shots have to be given in a doctor’s office because they can, though only rarely, provoke potentially fatal immune system reactions, called anaphylaxis. Also, to avoid such reactions, the dose used is started low and gradually increased over several months.
The sublingual treatments can cause throat irritation as well as itching and swelling in the mouth, but almost never anaphylaxis. So it is expected that, except for the initial dose, the treatments can be taken at home. And patients can start at the full dose immediately or almost immediately.
Still, some studies suggest that the sublingual therapy may not be quite as effective as injections. Also, the tablets contain only specific allergens, such as for grass; shots are customized by allergists to contain multiple extracts, such as for weeds, dust mites and so on, to match a patient’s allergies.
“It’s rare that somebody comes in and they are just allergic to one grass,” said Dr. Rohit K. Katial, professor of medicine at National Jewish Health in Denver. “Generally, people who are allergic tend to be allergic to multiple things.”
The companies have not said how much the drugs will cost, but some doctors think it will be about $150 a month. Oralair sells for about that much in Canada. Shots cost about $25 each, higher if they contain more allergens, according to Dr. Cox, who has been a consultant to Stallergenes and other companies.
Mark Schoenebaum, an analyst at ISI Group, projects that Merck’s tablets for grass and ragweed will have peak annual sales of about $350 million combined. That is not much for a giant like Merck, but it bolsters the company’s allergy and asthma business, which is suffering from generic competition to the blockbuster pill Singulair.
Another issue is whether patients will continue taking the daily tablets long enough to achieve lasting changes in their immune systems.
A recently published study from the Netherlands, which analyzed pharmacy records, found that only 7 percent of those getting sublingual immunotherapy completed the recommended three years of treatment. That was even worse than the 23 percent of patients getting allergy shots.
New approaches might help. “What we need is something that is very quick, a very short course, that has a long duration of effect,” said Dr. Mark Larché, a professor of medicine at McMaster University in Canada.
Dr. Larché is a co-founder of Circassia, a British company that is developing a therapy that would require as few as four monthly injections. It is now in the final phase of clinical trials as a treatment for cat allergies.
Another short-duration treatment that has shown promise consists of three monthly injections of the allergen into the lymph nodes in the groin.
Other treatments are being developed, but some have fallen by the wayside. The immune system is complex, as is nature. Some clinical trials have failed because the allergy season turned out to be so mild that even those getting the placebo had few symptoms.
Looking at the Sun Can Trigger a Sneeze
 PHOTIC SNEEZE: Crossed nerve signals in the brain may be the reason some people sneeze when exposed to a sudden bright light.
PHOTIC SNEEZE: Crossed nerve signals in the brain may be the reason some people sneeze when exposed to a sudden bright light.
Have you ever emerged from a matinee movie, squinted into the sudden burst of sunlight and sneezed uncontrollably? Up to a third of the population will answer this question with an emphatic “Yes!” (whereas nearly everyone else scratches their head in confusion). Sneezing as the result of being exposed to a bright light—known as the photic sneeze reflex—is a genetic quirk that is still unexplained by science, even though it has intrigued some of history’s greatest minds.
Aristotle mused about why one sneezes more after looking at the sun in The Book of Problems: “Why does the heat of the sun provoke sneezing?” He surmised that the heat of the sun on the nose was probably responsible.
Some 2 ,000 years later, in the early 17th century, English philosopher Francis Bacon neatly refuted that idea by stepping into the sun with his eyes closed—the heat was still there, but the sneeze was not (a compact demonstration of the fledgling scientific method). Bacon’s best guess was that the sun’s light made the eyes water, and then that moisture (“braine humour,” literally) seeped into and irritated the nose.
Humours aside, Bacon’s moisture hypothesis seemed quite reasonable until our modern understanding of physiology made it clear that the sneeze happens too quickly after light exposure to be the result of the comparatively sluggish tear ducts. So neurology steps in: Most experts now agree that crossed wires in the brain are probably responsible for the photic sneeze reflex.
A sneeze is usually triggered by an irritation in the nose, which is sensed by the trigeminal nerve, a cranial nerve responsible for facial sensation and motor control. This nerve is in close proximity to the optic nerve, which senses, for example, a sudden flood of light entering the retina. As the optic nerve fires to signal the brain to constrict the pupils, the theory goes, some of the electrical signal is sensed by the trigeminal nerve and mistaken by the brain as an irritant in the nose. Hence, a sneeze.
But because this harmless (albeit potentially embarrassing) phenomenon doesn’t seem to be linked with any other medical condition, scientific study of the subject has been scarce. Research has done little more than document its existence and attempt to gauge its prevalence. No rigorous studies exist, but informal surveys peg 10 to 35 percent of the population as photic sneezers. A study in the 1960s showed that the trait is autosomal-dominant—the gene is neither on the X nor Y chromosome and only one copy of the gene has to be present for the trait to be expressed—so if one parent sneezes when they look at a bright light, about half of his or her children will, too.
The genetic culprit remains unidentified, but scientists are starting to take an interest in trying to find out. “I think it’s worth doing,” says Louis Ptácek, a neurologist at the University of California, San Francisco, and an investigator at the Howard Hughes Medical Institute. Ptácek studies episodic disorders such as epilepsy and migraine headaches, and he believes that investigating the photic sneeze reflex could shed light on their related neurology.
Epileptic seizures are sometimes triggered by flashing lights and migraine headaches are often accompanied by photophobia. “If we could find a gene that causes photic sneezing, we could study that gene and we might learn something about the visual pathway and some of these other reflex phenomena,” Ptácek says.
But until he and his colleagues find the right families for their study, the photic sneeze reflex will remain something of a genetic novelty act, like the ability to roll your tongue. Although a 1993 paper in the journal Military Medicine raised concerns that light-induced sneezing might endanger fighter pilots, for whom a split second of lost vision could be lethal in certain situations, such fear was largely put to rest when a small study found that wearing sunglasses eliminated the effect.
Beyond that blip of gravitas, papers published about photic sneezing have largely leaned toward the whimsical end of the spectrum. Consider one 1978 publication that took advantage of the then-raging acronym fad and suggested an alternate name for the photic sneeze reflex: Autosomal-dominant Compelling Helio-Ophthalmic Outburst syndrome, or, of course, ACHOO.
Comprehensive Excellence
YOUR ONLY DESTINATION FOR COMPREHENSIVE EXCELLENCE
“One Doctor for One Nose”….
The Sinus and Allergy Center is focused exclusively on nasal, sinus, and allergy problems. We are board certified ear, nose, and throat surgeons. Dr. Todd had formal residency training and obtained fellowship accreditation in allergy and performs a high volume sinus and nasal surgery.
We offer state-of-the-art minimally invasive, image-guided sinus surgery, as well as unparalleled experience in rhinoplasty (plastic surgery of the nose) and nasal airway surgery.
We also offer comprehensive allergy testing and treatment, utilizing all the latest technology and techniques.
Our unique combination of skills, training, and experience allows the Sinus and Allergy Center to be the final consult for all your allergy, nasal, and sinus problems.
Pediatric Food Allergies
 Infants and Toddlers have a much more permeable GI tract and are very susceptible to food allergies. These can be difficult and can be mediated through both IgE and IgG. They can result in terrible GI symptoms of vomiting, diarrhea, bloating and colic. They can also result in skin symptoms such as atopic dermatitis and eczema or upper respiratory tract symptoms such as nasal congestion, ear and sinus infections. They lead to many sleepless nights for both the child and parents.
Infants and Toddlers have a much more permeable GI tract and are very susceptible to food allergies. These can be difficult and can be mediated through both IgE and IgG. They can result in terrible GI symptoms of vomiting, diarrhea, bloating and colic. They can also result in skin symptoms such as atopic dermatitis and eczema or upper respiratory tract symptoms such as nasal congestion, ear and sinus infections. They lead to many sleepless nights for both the child and parents.
The diagnosis is made primarily by taking a history. Your physician needs to be educated and aware food allergies. Unfortunately the allergy skin and blood tests are not very sensitive for IgG mediate (or cyclic) food allergies. A food diary for the child or nursing mother is paramount. IgG testing has not been proven helpful. It has often been called a very expensive means to a food diary. IgE blood testing and skin testing can be helpful and we do typically perform them here at Midwest ENT. Eosinophilic esophagitis is a new and disturbing end point for allergies affecting the gastrointestinal tract.
Treatment is primary dietary manipulation. We encourage mothers to continue nursing and actually monitor their own diet as many antigenic proteins pass through the breast milk. Casein and Whey are the primary antigenic proteins in Cow’s milk, and dairy is the biggest culprit. In children that are not nursing we often will try a hypoallergenic formula. Our favorites include Elecare, Neocate, and Neutramogen. They can be quite expensive and Neutramogen smells funny. I recommend buying them on E-Bay. EO28 Splash is another excellent option. Goats milk is a good alternative for some, Soy milk is excellent if they are not Soy allergic. Rice milk is also a good option.
Desensitization is controversial, however, we do now offer the LaCrosse protocol for our patients. This has proven extremely helpful for many of our patients and represents an exciting break through. The good news is that, with the exception of fixed food allergies (such as those to peanut), most children will outgrow these sensitivities. As the intestinal tract matures fewer proteins can cross and more foods will be tolerated. We can help you work through these trying times and offer you any and all possible treatments.
Chemical Middle Ear Treatments
What is it?
Chemical Perfusion (C.P.) is a new treatment for the application/delivery of specific medication(s) into the inner ear with the goal of curing or controlling diseases affecting the hearing and/or balance nerves and fluid pressures of the inner ear.
C.P. is a procedure which can be performed either in the office setting or at an outpatient surgical facility. The procedure is done alone or in conjunction with other “non-destructive” operations of the inner ear.
Indications
Presently chemical perfusion is used to control dizziness arising from diseases of the inner ear, e.g., Meniere’s disease, and for sudden deafness, severe tinnitus and cohlear hydrops. Depending on the inner ear disease being treated and its severity, medications currently used are: aminoglycosides (gentamicin), corticosteroids (dexamethasone) or anesthetics (lidocaine).
Points to remember. Anesthetics in the middle ear will lead to big time vertigo. Never do an ablative therapy in Meneire’s patients for 2-3 years as the propensity for bilaterality is real. Hearing must be followed carefully.
Technique
C.P. occurs with the application of a specific concentration of medication (the “chemical”) into the middle ear so that it can be transmitted (“perfused”) into the inner ear via the semi-permeable round window membrane separating the middle and inner ear compartments. A successful technique is the placement of a ventilation tube within the tympanic membrane and a microwick (which acts like a sponge) through the lumen of the tube. The wick extends through the middle ear to the round window membrane. Drops of the medication are placed into the ear canal at surgery, transferred by the wick, and absorbed through the round window membrane into the inner ear. Medication is then instilled on a daily basis by the patient for two to three weeks.
The patient is closely monitored pre- and post-operatively with serial hearing and balance tests as well as clinical examination until the desired result is attained. The desired result may be control of the dizziness, reversal or stabilization of the hearing loss or reduction of the tinnitus or fluid pressure.
Results
The most highly effective application of C.P. is in the treatment of Meniere’s disease, which has failed to respond to dietary and medical management. Its success rate is approaching 85 percent in controlling the disabling vertigo. The risk to hearing is less than 15 percent. It is, therefore, a valuable addition to the treatment of Meniere’s disease.


