 Until recently, esophageal eosinophilia was primarily attributed to acid reflux esophagitis. However, in the last five years, eosinophilic esophagitis—also known as allergic esophagitis, primary eosinophilic esophagitis, and idiopathic eosinophilic esophagitis—has emerged as an important independent issue found to occur in children and in adults.
Until recently, esophageal eosinophilia was primarily attributed to acid reflux esophagitis. However, in the last five years, eosinophilic esophagitis—also known as allergic esophagitis, primary eosinophilic esophagitis, and idiopathic eosinophilic esophagitis—has emerged as an important independent issue found to occur in children and in adults.
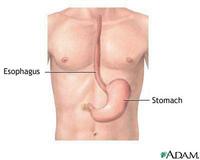
Eosinophilic esophagitis is a disease in which upper intestinal symptoms are associated with dense eosinophilic infiltration of the squamous esophageal epithelium or deeper esophageal tissue; neither symptoms nor eosinophilia respond to the administration of a proton pump inhibitor ( PPI). The pathophysiologic mechanisms are likely related to allergic inflammation, not to an underlying motility defect as in gastroesophageal reflux disease (GERD).
Typically allergies affect your upper respiratory tract with itchy watery eyes, sneezing, and rhinorrhea. Often they can contribute to lower airway issues such as asthma and cough. Secondly, they can lead to dermatologic manifestations such as exzema, dermatitis, and urticaria.
Eosinophilic esophagitis seems to be a manifestation of allergic disease on the digestive system. For years, the digestive system has been manifesting allergic inflammation in more subtle ways, but this disease should not be ignored. Treatment includes proton pump inhibitors, swallowed fluticasone (without the spacer), swallowed antifungals, and intermittent systemic steroids. Comprehensive allergy testing and immunotherapy have proven effective.
Singulair, carafate, and chromolyn may be helpful. Xolair and IL-5 inhibitor are still experimental. Food allergy testing is always completed and elimination diets are considered. A trial of an elemental amino acid diet may be entertained, but is rarely practical. Food drops or shots are still being studied.