Nasal Surgery
Subtle Nasal Surgery
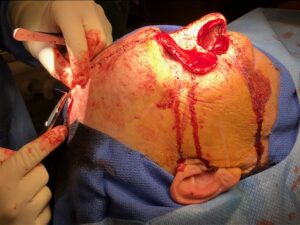
Resection and Reconstruction of a Nasal Cancer
The Perfect Nose
The Perfect Nose
Subtle Reduction Rhino
Ramsay Hunt Syndrome (Type 2)
James Ramsay Hunt (1872-1937) was a famous Neurologist who named a number of things. The most known is Type 2, the reactivation of herpes zoster in the geniculate ganglion. It is sometimes called herpes zoster oticus, and has variable presentation which may include a lower motor neuron lesion of the facial nerve, deafness, vertigo, and pain. A triad of ipsilateral facial paralysis, ear pain, and vesicles on the face, on the ear, or in the ear is the typical presentation.
This young lady is 2 weeks out from a varicella vaccination. We treated her successfully with Valtrex and Prednisone. More questions than answers here.
Malignant Otitis Externa
Necrotizing external otitis
Necrotizing external otitis (malignant otitis externa) is an uncommon form of external otitis that occurs mainly in elderly diabetics, being somewhat more likely and more severe when the diabetes is poorly controlled. Even less commonly, it can develop due to a severely compromised immune system. Beginning as infection of the external ear canal, there is an extension of the infection into the bony ear canal and the soft tissues deep to the bony canal. Unrecognized and untreated, it may result in death. The hallmark of malignant otitis externa (MOE) is unrelenting pain that interferes with sleep and persists even after swelling of the external ear canal may have resolved with topical antibiotic treatment.[18] It can also cause skull base osteomyelitis (SBO), manifested by multiple cranial nerve palsies, described below under the “Treatment” heading.
Natural history
MOE follows a much more chronic and indolent course than ordinary acute otitis externa. There may be granulation involving the floor of the external ear canal, most often at the bony-cartilaginous junction. Paradoxically, the physical findings of MOE, at least in its early stages, are often much less dramatic than those of ordinary acute otitis externa. In later stages, there can be soft tissue swelling around the ear, even in the absence of significant canal swelling. While fever and leukocytosis might be expected in response to bacterial infection invading the skull region, MOE does not cause fever or elevation of white blood count.
Treatment of MOE
Unlike ordinary otitis externa, MOE requires oral or intravenous antibiotics for cure. Pseudomonas is the most common offending pathogen. Diabetes control is also an essential part of treatment. When MOE goes unrecognized and untreated, the infection continues to smolder and over weeks or months can spread deeper into the head and involve the bones of the skull base, constituting skull base osteomyelitis (SBO). Multiple cranial nerve palsies can result, including the facial nerve (causing facial palsy), the recurrent laryngeal nerve (causing vocal cord paralysis),[citation needed] and the cochlear nerve (causing deafness).
The infecting organism is almost always pseudomonas aeruginosa, but it can instead be fungal (aspergillus or mucor). MOE and SBO are not amenable to surgery, but exploratory surgery may facilitate the culture of unusual organism(s) that are not responding to empirically used anti-pseudomonal antibiotics (ciprofloxacin being the drug of choice). The usual surgical finding is diffuse cellulitis without localized abscess formation. SBO can extend into the petrous apex of the temporal bone or more inferiorly into the opposite side of the skull base.[citation needed]
The use of hyperbaric oxygen therapy as an adjunct to antibiotic therapy remains controversial.[18]
Complications
As the skull base is progressively involved, the adjacent exiting cranial nerves and their branches, especially the facial nerve and the vagus nerve, may be affected, resulting in facial paralysis and hoarseness, respectively. If both of the recurrent laryngeal nerves are paralyzed, shortness of breath may develop and necessitate tracheotomy. Profound deafness can occur, usually later in the disease course due to relative resistance of the inner ear structures. Gallium scans are sometimes used to document the extent of the infection but are not essential to disease management. Skull base osteomyelitis is a chronic disease that can require months of IV antibiotic treatment, tends to recur, and has a significant mortality rate.[18]
Apical Petrousitis—Gradenigo’s Syndrome
Gradenigo’s syndrome, also called Gradenigo-Lannois syndrome, is a complication of otitis media and mastoiditis involving the apex of the petrous temporal bone. It was first described by Giuseppe Gradenigo in 1904.

Symptoms
Components of the syndrome include:
- retroorbital pain due to pain in the area supplied by the ophthalmic branch of the trigeminal nerve (fifth cranial nerve),
- abducens nerve palsy (sixth cranial nerve)
- otitis media
Other symptoms can include photophobia, excessive lacrimation, fever, and reduced corneal sensitivity. The syndrome is classically caused by the spread of an infection into the petrous apex of the temporal bone.
Diagnosis
The constellation of symptoms was first described as a consequence of severe, advanced ear infection which has spread to a central portion of the temporal bone of the skull. This type of presentation was common prior to development of antibiotic treatments, and is now a rare complication.
In persons with longstanding ear infection and typical symptoms, medical imaging such as CT or MRI of the head may show changes that confirm disease involvement of the petrous apex of temporal bone.
Treatment
The medical treatment is done with antibiotics: ceftriaxone plus metronidazole (which covers anaerobic bacteria). In more severe cases, a paracentesis (aspiration of fluids) or mastoidectomy may be needed.
Eponym
It is named after Count Giuseppe Gradenigo, an Italian Otolaryngologist, and Maurice Lannois.