Chronic Cough
 A cough is a protective, primitive reflex in healthy individuals. It serves to expectorate unwanted substances from the upper respiratory tract. A persistent cough can be debilitating, socially distressing, and adversely impair quality of life. One of the more common presentations to a medical practitioner is a dry cough.
A cough is a protective, primitive reflex in healthy individuals. It serves to expectorate unwanted substances from the upper respiratory tract. A persistent cough can be debilitating, socially distressing, and adversely impair quality of life. One of the more common presentations to a medical practitioner is a dry cough.Causes
A cough begins when an irritant — stomach acid, mucus, hair spray, perfume, even spicy food — stimulates nerves in your respiratory tract. The cough impulse travels to your brain, which then signals muscles in your stomach and diaphragm to give a strong push to air in your lungs. It takes such force to expel irritants that the speed of coughed air can approach 500 miles an hour.
An occasional cough is normal — it helps clear foreign substances and secretions from your lungs and prevents infection. But a cough that persists for long periods of time is usually the result of an underlying problem, such as:
- Postnasal drip. Every day, glands in your nose and throat produce a quart or two of mucus, which cleans and moisturizes your nasal passages. Normally, you swallow the fluid without knowing it, but when there’s more than usual — from allergies, a cold or sinus infection — you may feel it accumulating in the back of your throat. This excess mucus, commonly called postnasal drip, can cause irritation and inflammation that trigger your cough reflex. If the postnasal drip is chronic, your cough is likely to become chronic, too. Though postnasal drip is often obvious, it’s possible to have the condition without ever having symptoms.
- Asthma. This is a common cause of chronic cough in adults and the leading cause in children. Most often, the cough occurs with wheezing and shortness of breath, but in one type of asthma, cough is the only symptom. This is sometimes termed cough variant asthma (CVA). An asthma-related cough may come and go with the seasons, appear after an upper respiratory tract infection, or become worse when you’re exposed to cold air or certain chemicals or fragrances.
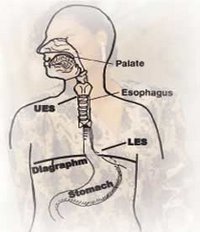
- Gastroesophageal reflux disease (GERD). In this common condition, stomach acid flows back into the tube that connects your stomach and throat (esophagus). The constant irritation in your esophagus, throat and even your lungs can lead to chronic coughing. Acid reflux often causes heartburn and a sour taste, yet close to half the people whose cough is due to reflux have no symptoms.
- Respiratory tract infection. A cough can linger long after most symptoms of a cold, flu, pneumonia or other infection of the upper respiratory tract have gone away. This may be because the airways remain inflamed and therefore especially sensitive to irritants. This is probably the most common etiology and has in the past been termed the “100 days cough”.
- Blood pressure drugs. Angiotensin-converting enzyme (ACE) inhibitors, which are commonly prescribed for high blood pressure and heart failure, are known to cause chronic cough in about 20 percent of the people taking them. Most often, the cough begins within a week of starting therapy, but it sometimes may not develop for up to six months. And though the cough usually goes away a few days after the drug is stopped, it can linger for a month or more. Aspirin and beta blockers have also been implicated in chronic cough. They can increase the airway “twitchiness” and make allergy treatment more problematic.
- A laryngeal lesion. Sometimes a lesion such as a polyp, nodule, or even a cancer can precipitate a cough.
- Chronic bronchitis. This long-standing inflammation of your major airways (bronchial tubes) can cause congestion, breathlessness, wheezing and a cough that brings up discolored sputum. Because most people with chronic bronchitis are current or former smokers, the cough is usually a sign of damage to the lungs and airways.
- Infection. Exposure to perhaps an atypical agent such as mycoplasma or acid fast organism such as mycobacteria tuberculosis must always be considered.
- Bronchiectasis. This is a serious, chronic lung condition in which abnormal widening of your bronchial tubes affects their ability to clear mucus from your lungs. Signs and symptoms include a cough that may bring up discolored sputum or blood, shortness of breath and fatigue.
- Foreign Body. More commonly in kids, the aspiration of a foreign body can lead to a chronic irritation and cough.
- Lung cancer. Only a small percentage of people with a chronic cough have lung cancer, and most are current or former smokers. If you smoke now, smoked at one time or your sputum contains blood, see your doctor.
- Habit or psycogenic Cough. Many times coughing or clearing the throat can become a habit and is actually propogated by the individual. These coughs usually abate at night when the person is sleeping where as physiologic cause will usually persist and awaken the patient.
Risk factors
Anyone can develop a chronic cough, but these factors make you more susceptible:
- Smoking. Being a current or former smoker is one of the leading risk factors for chronic cough. A “smoker’s cough” is often a warning sign of emphysema, a disease that causes ongoing and irreversible damage to your lungs. Frequent exposure to secondhand smoke also can lead to coughing and lung damage.
- Your sex. Because women tend to have more sensitive cough reflexes than men do, they’re more likely to develop a chronic cough.
- Allergens. Ongoing exposure to allergens such as dust, pollen, pet dander, cleaning products and chemical fumes can cause a persistent cough, even in people who don’t ordinarily have allergies or asthma.
- Pollution. Environmental pollutants such as diesel exhaust, ozone and nitrogen dioxide are leading causes of chronic coughing in both children and adults.
Screening and diagnosis
A thorough medical history and physical exam can provide important clues about a chronic cough. Tell your doctor if you take blood pressure medication, smoke or are routinely exposed to environmental pollutants. Using this information, your doctor may try to determine the cause of your cough based on your response to treatment rather than on test results.
For instance, if your doctor suspects that your cough is the result of postnasal drip, you’re likely to be given an antihistamine-decongestant medication. If your cough goes away, the diagnosis is confirmed. When this approach fails, or you become frustrated with the trial-and-error process, you may have one or more of the following tests:
- Allergy Testing. If you and your doctor suspect that postnasal drip or allergy is causing your cough, then allergy testing can be important. We offer both skin and blood testing at Midwest Ear, Nose, and Throat. We also offer all forms of allergy management: Avoidance, Medications, and both shot and sublingual immunotherapy.
- Sinus Evaluation: You might also have a Nasal Endoscopy and or computerized tomography (CT) scan of your sinuses to check for infection. The physicians at Midwest Ear, Nose, and Throat have the highest level of training and experience in sinonasal disorders.
- Chest X-ray and PPD. Although a routine chest X-ray won’t reveal the most common reasons for a cough, such as postnasal drip or GERD, it may be used to check for lung cancer and other lung diseases. If the test reveals something that requires further study, your doctor might recommend a CT scan, a computerized X-ray that shows your lungs in far greater detail than conventional X-rays do.
- Lung function tests. These simple, noninvasive tests measure how much air your lungs can hold and how quickly you can inhale and exhale. Sometimes you may also have an asthma challenge test, which tests your breathing before and after inhaling a drug called methacholine. If you have asthma, you’ll have a harder time breathing after inhaling the methacholine.
- Endoscopy. Your doctor may use a test called an esophagogastroduodenoscopy (EGD) to check for signs of acid reflux disease. During the test, a thin, flexible tube equipped with a light and camera (endoscope) is placed down your throat. The endoscope allows your doctor to check for ulcerations and inflammation in your esophagus and stomach. This can be done at Midwest Ear, Nose, and Throat with a small scope place through the nose.
- Bronchoscopy. If your cough persists and the cause remains uncertain, your doctor may recommend bronchoscopy, a procedure in which a flexible, lighted tube is placed through your windpipe into your bronchial tubes. This can help diagnose certain kinds of lung cancer, infection, bronchitis, and objects that might be lodged in your breathing tubes. The physicians at Midwest Ear, Nose, and Throat are trained in both ridgid and flexible bronchoscopy.
- pH probe. To help diagnose acid reflux, your doctor may use a test called a pH probe. This involves placing a tube through your nose or attaching a device to the wall of your esophagus during endoscopy to check for acid washing up into your esophagus. This test is available at our office.
Complications
Having a persistent cough can be physically exhausting, both because it requires so much energy to cough and because the cough often prevents you from sleeping well. A chronic cough can also cause:
- Headache
- Dizziness
- Excessive sweating
- Urinary incontinence0020
- Fractured ribs, especially in women with fragile bones
But coughing’s biggest toll may be social. Many chronic coughers say that going out in public simply becomes too embarrassing — all those looks of disgust in restaurants and theaters — and that their spouse or partner often ends up moving out of the bedroom. The result is increasing isolation, frustration and anger, not just for the cougher but sometimes for friends and family, too.
Treatment
Treating a chronic cough with a known cause is usually straightforward; when the cause can’t be determined, treatment becomes more problematic and frustrating. Depending on the reason for your cough, your doctor may prescribe:
- Allergy treatment. The standard treatment for allergies and postnasal drip, antihistamines and decongestants are usually given in combination. Older, sedating antihistamines may be more effective in treating cough than the newer generation of drugs that don’t make you drowsy. Other treatments for allergies and postnasal drip include nasal corticosteroids and nasal antihistamines. If those measures are insufficient then consideration of immunotherapy (allergy shots) is in order.
- Inhaled corticosteroids. These anti-inflammatory drugs are the most effective treatment for asthma as well as for asthma-related cough. They work by reducing inflammation in your airways. In some cases, you may also need a short course of oral corticosteroids. Although inhaled corticosteroids have a lower risk of side effects than oral corticosteroids do, long-term use may increase the risk of skin thinning, bruising, osteoporosis and cataracts. In children, they can slow growth slightly, but most children eventually reach their full height.
- Lifestyle changes. A cough caused by acid reflux can often be treated with lifestyle changes alone. These include maintaining a healthy weight; eating smaller, more frequent meals; avoiding heartburn triggers such as alcohol, chocolate, mint and fried foods; waiting three to four hours after a meal before lying down; and raising the head of your bed. Although these measures are usually effective, it may take months before your cough clears completely.
- Medications to treat acid reflux. When lifestyle changes don’t take care of acid reflux, you may be treated with a proton pump inhibitor, which blocks acid production and allows esophageal tissue time to heal. Prescription-strength proton pump inhibitors include esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix) and rabeprazole (Aciphex). They are generally safe, even when taken long term. To prevent possible side effects, such as stomach or abdominal pain, diarrhea and headaches, your doctor is likely to prescribe the lowest effective dose.
- Medication change. If your cough is caused by angiotensin-converting enzyme (ACE) inhibitors, switching to another type of medication may provide relief.
- Smoking cessation. The best treatment for chronic bronchitis is to stop smoking. Talk to your doctor about a comprehensive smoking cessation program that includes social support, nutritional counseling, nicotine gum or patches, and other medications.
- Medications or surgical intervention for Chronic Rhinosinusitis. Sometimes the condition of the nose and sinuses needs to be aggressively dealt with to lessen inflammatory post nasal drainage.
Other treatments. When the reason for your cough isn’t known, your doctor may prescribe a cough suppressant or possibly ipratropium bromide (Atrovent), a type of medication called a bronchodilator that relaxes the air passages in your lungs. Inhaled corticosteroids are sometimes used, though it’s not clear that they’re effective for a cough unrelated to asthma. Singulair, a leukotriene inhibitor, is often helpful in cough variant asthma. The physicians at Midwest Ear, Nose, and Throat can help the patient work through this frustrating condition.